Why digital medicine depends on interoperability
Published in Healthcare & Nursing
Explore the Research
Why digital medicine depends on interoperability - npj Digital Medicine
npj Digital Medicine - Why digital medicine depends on interoperability
The vast amounts of digital data collected in hospitals, medical practices, research labs or personal health apps have huge potential for medicine and healthcare. Unfortunately, these data are currently not used to their full potential. A major barrier is a lack of interoperability: Large parts of today’s health data are hidden in isolated databases and proprietary systems that do not talk to each other (or speak different languages). To turn data into meaningful information, we need standard formats and vocabularies for data exchange.
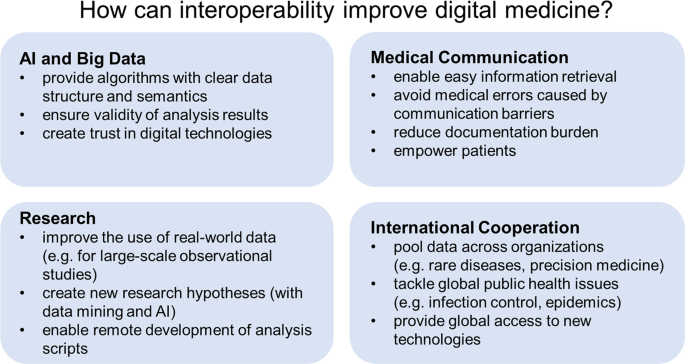
To bring the important topic of interoperability to the attention of readers interested in digital medicine, we wrote the paper “Why digital medicine depends on interoperability”. (Healthcare professionals are often not aware of this topic or fail to notice why it is so important.) Our paper discusses how interoperability can improve medicine. We focus on four areas where interoperability is particularly relevant:
1) Interoperability for artificial intelligence and big data
The quality of artificial intelligence (AI) and big data technologies depends on the data they are using. Training machine learning algorithms works best with structured data with clear labels. International standards and terminologies can provide algorithms with the data necessary for building powerful AI algorithms.
2) Interoperability for medical communication
Interoperable data improve information retrieval, providing clinicians with the information they need to provide optimal care for their patients. This can help to avoid medical errors and reduce the documentation burden of physicians. It can also give patients a more complete picture of their data, helping them to take a more active role in managing their health and well-being.
3) Interoperability for research
Interoperability can also improve research. Standard formats and terminologies can make large amounts of disconnected real-world data accessible to research and enable the remote development of analysis scripts.
4) Interoperability for international cooperation
Finally, interoperability in medicine and healthcare makes it possible to pool data across institutional, regional and national boundaries. This can foster international collaboration, for example in areas of rare diseases, precision medicine or infection control. International standards for the exchange of health data also facilitate the global dissemination of new technologies.
We hope that our paper motivates healthcare professionals to think about the importance of interoperability in their own work. Ultimately, improving interoperability will help to achieve the full potential of digital medicine to provide optimal care to patients.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in