A Crisis, A Question, A Program: The Story Behind the PRMD Moral Distress Intervention
Published in Healthcare & Nursing
The Story Behind the Paper
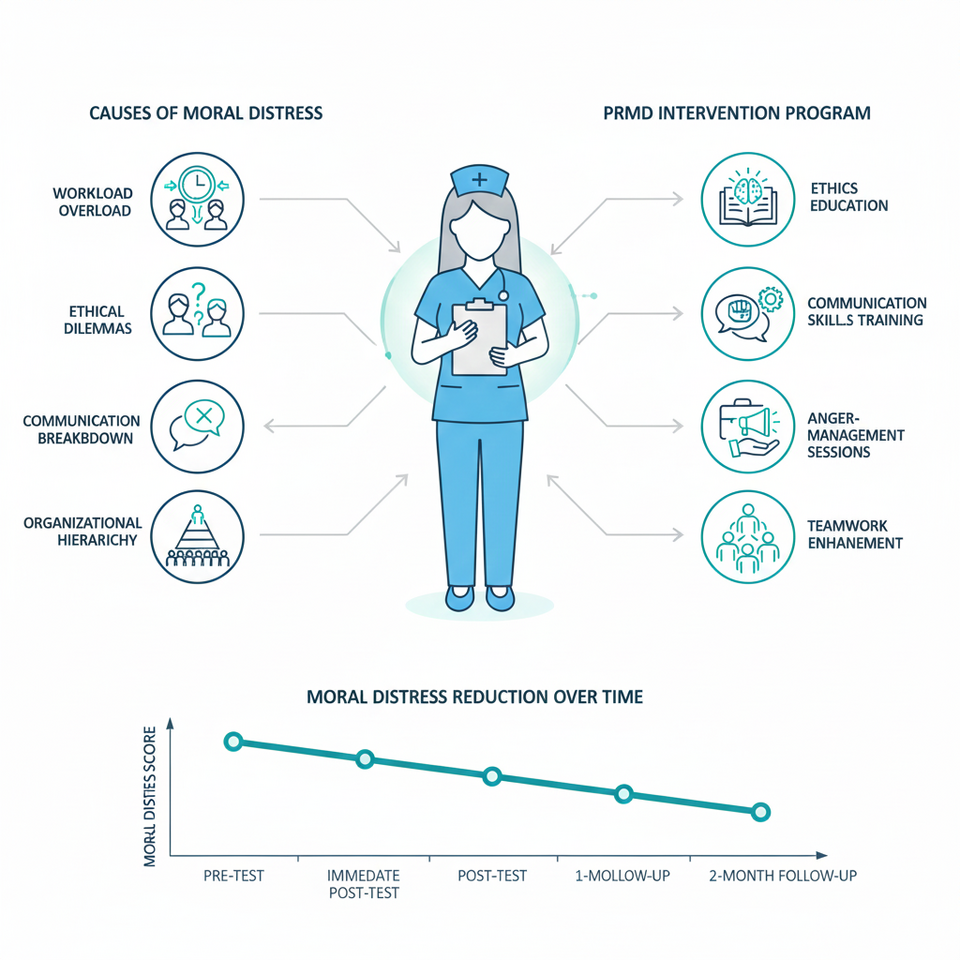
During the COVID-19 pandemic, Iranian hospitals—especially psychiatric wards—became arenas of intense ethical tension. Nurses found themselves trapped between knowing the morally right action and being unable to carry it out because of staff shortages, organizational constraints, overwhelming workloads, or conflicting orders. We witnessed skilled and compassionate nurses experiencing guilt, frustration, powerlessness, and emotional exhaustion as ethical dilemmas multiplied around them.
These real-world challenges raised an urgent question for us:
Why do Iranian nurses experience persistent moral distress, and what kind of intervention—rooted in local culture, conditions, and organizational realities—can truly alleviate it?
Through interviews with front-line nurses, we repeatedly heard stories of unfair workload distribution, poor communication across teams, aggressive patient behavior, hierarchical cultures that silenced nurses, and direct exposure to ethically troubling situations. These encounters were the spark that motivated us to design a structured, culturally grounded program to reduce moral distress.
Conceptual Framing—Bringing Theory to Life
Our study drew upon three guiding perspectives:
-
Professional Nursing Ethics: Highlighting how ethical knowledge, moral sensitivity, decision-making skills, and institutional support can strengthen nurses’ moral resilience.
-
Pragmatic Educational Philosophy: Emphasizing that ethics cannot be taught only through lectures; it must be practiced and reflected upon through real cases, storytelling, and interactive learning.
-
A Multidisciplinary Lens: Integrating medical ethics, nursing management, communication science, and program planning to create a multi-layered intervention.
Our premise was clear:
Moral distress is not caused by a single deficit. It is the result of interconnected individual, managerial, organizational, and relational factors. Only a multi-dimensional intervention can meaningfully reduce it.
Methodology – Systematic Design of an Educational Intervention
To explore this complexity and design a suitable solution, we adopted a multiphase mixed-methods design:
-
Qualitative Phase:
Interviews with 12 nurses revealed the roots of moral distress—deficient professional competency, inadequate communication, hierarchical organizational culture, high workload, poor task allocation, personal ethical uncertainty, and witnessing moral dilemmas. -
Program Design (PRMD):
Using the Ewles & Simnett Model, we developed an intervention that combined educational, managerial, and environmental strategies. Ethics workshops, case-based discussions, communication training, anger-management sessions, moral storytelling, and virtual learning activities were incorporated. -
Program Implementation:
Forty nurses participated in the 3-month program, which included face-to-face classes, virtual sessions, ethics discussions, managerial meetings, and scenario-based exercises. -
Program Evaluation:
Using a pre-test and repeated post-tests alongside a secondary qualitative phase, we assessed the program’s effects at four intervals.
This structured, evidence-driven process allowed us to design a culturally consistent program grounded in both empirical data and practical realities.
Key Findings—What the Evidence Revealed
-
A significant reduction in moral distress:
Quantitative results showed a steady, meaningful decline in the frequency, intensity, and total moral distress scores immediately after the intervention and at one- and two-month follow-ups. -
Moral empowerment of nurses:
Nurses reported improved ethical awareness, stronger decision-making abilities, greater confidence, and a clearer understanding of ethical principles. -
Enhanced ethical climate:
Better workload management, improved task allocation, and greater managerial involvement contributed to a more supportive, fair, and ethical work environment. -
Improved communication and teamwork:
Through discussions, scenario-based learning, and communication training, nurses experienced better interactions with colleagues and patients.
Together, these findings showed that moral distress is not simply an emotional burden—it is shaped by education, culture, management, and workplace structures.
Why This Matters—The Iranian Nursing Lens
Iran’s health system faces chronic nursing shortages, heavy workloads, and hierarchical clinical cultures. Existing international moral distress interventions do not align with local realities: they overlook cultural norms, resource limitations, and ethical expectations specific to Iranian nurses.
Our study is rooted in Iranian nurses’ lived experiences and responds directly to their needs. The PRMD program is one of the first comprehensive, evidence-based, and culturally adapted interventions for reducing moral distress in Iran.
Policy and Practice Implications—Beyond Education
One message is clear:
Moral distress cannot be reduced through education alone. Organizational transformation is essential.
We recommend:
-
Meaningful participation of nurses in clinical and managerial decision-making
-
Establishment of active ethics committees in hospitals
-
Continuous ethics education with real cases and scenarios
-
Redesigning task allocation and workload systems
-
Strengthening interprofessional communication
-
Managerial engagement in creating an ethical climate
These changes can elevate ethical quality, reduce emotional burden, and enhance the well-being of nurses and patients alike.
Why the Timing Matters
Published in 2023, this paper emerged in the aftermath of COVID-19, when nurses had endured unprecedented ethical pressures. The timing is critical: the health system must now rebuild not only its physical capacity but also the moral and psychological resilience of its frontline workforce.
Personal Motivation – A Moral Commitment
For us as researchers, this project was more than an academic endeavor—it was a moral obligation. Iranian nurses navigate complex ethical landscapes with limited support, yet they continue to strive for compassionate and just care. Many shared their pain quietly, without institutional recognition or emotional support.
We felt responsible for amplifying their voices, translating their struggles into evidence, and creating a pathway toward meaningful change.
Conclusion
This study builds bridges between nursing ethics, healthcare management, education, and organizational justice.
We hope it inspires broader conversations and future action towards a workplace where:
no nurse stands alone in ethical distress.
no moral dilemma goes unaddressed.
and ethical practice becomes a shared, supported responsibility.
Follow the Topic
-
BMC Medical Education

This is an open access journal publishing original peer-reviewed research articles in relation to the education and training of healthcare professionals. It welcomes studies on students and professionals across all levels of education; education delivery aspects; and other education-related topics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Artificial intelligence in curriculum development and assessment
BMC Medical Education welcomes submissions to our Artificial intelligence (AI) in curriculum development and assessment Collection. The incorporation of AI technologies and methodologies into medical and allied health curricula and student assessment is not just a trend, but a crucial step towards improving program effectiveness and producing efficient and professional doctors and allied health professionals. This Collection aims to explore how AI is reshaping medical and allied health curricula, student training, and assessment, as well as the potential implications of these changes on healthcare services and patient wellbeing.
Research on AI in medical education is still in its early stages. However, there has been a marked increase in interest and activity in this area during 2023 and 2024. Still, the majority of existing publications are commentary articles, perspective pieces, letters to the editor, or editorials, rather than original research. This highlights the pressing need for rigorous research and systematic reviews on the application of AI in medical education. Additionally, most contributions come from countries such as the United States, Canada, the United Kingdom, Australia, China, Singapore, Denmark, and Oman. In contrast, there is a significant underrepresentation of research output from regions including North Africa, the Middle East, South-East Asia, and South America.
This new Collection focuses specifically on curriculum development and student assessment, and researchers are encouraged to submit their work for consideration. Continued exploration in this domain has the potential to revolutionize medical education and, ultimately, enhance patient care worldwide. This reflects the transformative power of AI in shaping the future of medical training.
Submissions of innovative research contributing to this goal are invited. The scope of this Collection includes, but is not limited to, the following topics:
• Validity and reliability of AI in curriculum development
• AI applications in student selection and the allocation of medical and allied health graduates into specialties and subspecialties
• The use of AI in developing assessment questions and marking essay questions
• The potential of AI in marking OSCE examinations
• AI applications in providing performance feedback to students
• Critical assessment of AI-performed tasks in curriculum design and in student evaluation
• Validity and accuracy of AI-generated clinical cases
• Utilization of AI in faculty development and continuing medical education
• Students’ use of AI in learning environments
• Critical analysis of AI-generated responses and outputs
• Evaluation of published research on AI’s role in assessment and question design
Contributions are welcomed from a range of disciplines, including healthcare professionals, medical educators, social scientists, and computer scientists. The Collection also seeks submissions from fields such as dentistry, pharmacy, nursing, physiotherapy, occupational therapy, speech pathology, psychology, midwifery, oral therapy, paramedicine, and optometry. The goal is to build a vibrant, interdisciplinary Collection that captures the latest developments and research on AI's impact in curriculum and assessment within medical and allied health education.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 4: Quality Education.
Publishing Model: Open Access
Deadline: Mar 02, 2026
Tools for assessment of medical skills
BMC Medical Education is calling for submissions to our Collection on Tools for assessment of medical skills. Effective assessment is essential for ensuring that future health professionals trainees develop the skills required for safe and competent practice. From objective structured clinical examinations (OSCEs) and workplace-based assessments to simulation-based evaluations and real-time feedback methods, advancements in assessment tools are shaping the future of medical education. As medical training evolves, integrating reliable and valid professional evaluation techniques is crucial to fostering competency-based education and lifelong learning and ensuring optimal future professional performance.
We welcome research covering topics such as, but not limited to:
• Development and validation of novel assessment tools in medical education
• Technology-enhanced assessments, including artificial intelligence and virtual simulation
• Formative assessments and feedback methods to support skill acquisition
• Objective structured clinical examinations (OSCEs) and standardized patient assessments
• Workplace-based assessment strategies for clinical competency evaluation
• Best practices in professional evaluation for medical learners and educators
• Documentation of curricular innovations or integrations with a focus on assessment
This Collection seeks to advance the field of medical education by promoting evidence-based strategies for assessing and improving medical skills. By exploring innovative and practical approaches to evaluation, we can enhance both learning outcomes and patient care.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 4: Quality Education.
Publishing Model: Open Access
Deadline: Mar 12, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in