A fast-forming non-swelling hydrogel
Published in Bioengineering & Biotechnology

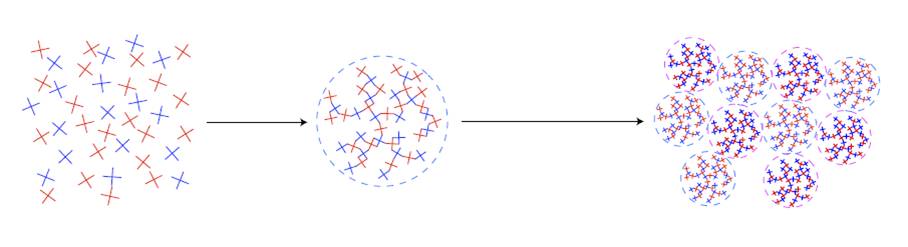
My advisor, Prof. Sakai, wanted to come up with a polymer hydrogel that formed fast in the disadvantageous gelation conditions of low polymer concentration. Yet the prepolymers that he could use had an insufficient degree of reactivity at low concentration. To resolve this challenge, we came up with an original idea. We divided the typical gelation process into two steps. In the first step, hyper-branched polymeric clusters are formed by intentionally stopping the gelation reaction prior to the gelation point. Through this process, we can control the distance from the gelation point. In the second step, instead of the prepolymer, we used the polymeric clusters formed by the first process (Figure). This split of the gelation process into two steps makes it possible to shorten the gelation time regardless of the reactivity of the prepolymers.
In clinical practice, injectable hydrogels are needed, and these have to gel in an appropriately short time. Another important requirement is for the hydrogel’s swelling pressure to be appropriately low. This is because swelling in vivo induces compression in surrounding tissues and potentially the failure of the implanted material, which can then cause serious adverse reactions. One of the effective ways to suppress the swelling pressure is to prepare a hydrogel at a low concentration. However, the gelation time is unacceptably high at low polymer concentrations. We needed to accelerate the gelation time under this challenging condition. On the basis of our experiments, our two-step gelation process enabled us to form gels at a low concentration in a short time and with swelling pressure lower than the elastic modulus of soft tissue.
Professors Hoshi and Okamoto, who are ophthalmologists at Tsukuba University, became interested in our work after we discussed it at a conference, and this led to a collaboration about using the hydrogels as artificial vitreous bodies. I was really surprised and pleased when our hydrogel avoided retinal detachment in rabbit eyes. I hope that this hydrogel improves current surgery for retinal detachment, and increases the quality of life of patients.
Our system is based on a simple principle: tuning the gelation time by controlling the distance from the gelation point. This principle is versatile, and thus applicable to other gelation systems. Low swelling pressure and fast-formation in hydrogels were thought to imply a trade-off. I hope that our methodology breaks this trade-off, and opens up the synthesis of new hydrogel systems for biomedical applications.
Our paper: Hayashi, K. et al. Fast-forming hydrogel with ultralow polymeric content as an artificial vitreous body. Nat. Biomed. Eng. 1, 0044 (2017).




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Ms. Hayashi:
There are a slew of patients suffering from a minor ocular problem such as vitreous opacities. It might not seem to be even a disease to most of ophthalmologist considering it as a normal aging process. However,to patients suffering sympathetic vitreous opacities, their quality of life is dramatically reduced by floaters. The only efficacious treatment for the time being is vitrectomy which is a major operation carrying a list risk profile. The artificial vitreous seems to be a more promising replacement of vitreous than BSS so as a patient who had been by vitrectomy,I hope you can answer some questions and I really appreciate.
1.When will it become in clinical trial as you estimate or it has already been in clinical trial?
2.Is this kind of artificial vitreous similar to our nature born vitreous anatomically? As for now,we know the acceleration of cataract post vitrectomy is much likely due to the increasing oxygen partial pressure near lens which is carried in during operation. Will this kind of low concentration hydrogel provide better protection against lens' oxidation than BSS did.
3.As your thesis stated,it's much likely to be used against retinal detachment by injecting this hydrogel to reattach detached retina without intraocular surgery. Is there any chance the hydrogel becoming the major replacement of vitreous in vitro-retinal surgery for all pathology including vitreous opacities?
4.No observable adverse effect in rabbit experimet for 410 days. Do you have any ideas about the probable long term effects or this kind of hydrogel is very safe and almost without cytotoxicity as you expect?
5.How long will it take to spread out in east Asia after clinical trial in Japan or the time course is too hard to estimate?
6.In case of vitrectomy for floaters, there are debris such as inflammation cell ,blood cell,or residue vitreous left to be absorbed.In your evaluation,will this hydrogel stuck those debris in the cavity between Oligo-Tetra-PEG or deflat them out to touch eye ball which might accelerate the absorption?
Thanks,
Eric Yu-Chen Fuh
Taiwan