A single wearable sensor combined with machine learning estimates step length in older adults and patients with neurological disorders
Published in Social Sciences, Bioengineering & Biotechnology, and Neuroscience
Multi-disciplinary collaborations have long been viewed as an ideal approach for tackling challenging problems. The work described in our paper illustrates an example of this. In particular, a graduate student in biomedical engineering joined forces with an industrial engineering professor with expertise in machine learning, a professor in neuroscience and physical therapy, and experts in related fields to improve the ability to accurately estimate step length from a single, wearable sensor. Step length is a key, non-invasive marker of aging, many neurological disorders, and, often, disease progression. Just imagine the walking pattern of an aging grandparent or other family member. One of the noticeable characteristics is the relatively short steps, i.e., a reduced step length.
Conventional methods for quantifying step length include camera-based systems and instrumented gait mats. These methods are accurate; however, they only provide a snapshot view of a person’s walking at a given instant in time and may be biased by numerous factors (e.g., time of day, mood, and motivation), giving an incomplete description of an individual’s step length.
Inertial measurement units (IMUs) are electronic devices that measure accelerations and angular velocities. IMUs are lightweight, inexpensive, and ubiquitous. Nowadays, IMUs can be found in smartphones, smartwatches, and shoe insoles, as well as in dedicated sensors placed at different locations on the body. Thus, IMUs can be used in clinical settings and applied to assess real-world walking over an extended period of time (e.g., 24/7). Previous studies that aimed at estimating step length using IMUs were based on a relatively small, homogeneous group of subjects, focused on people without gait disturbances, involved inconvenient locations of the IMU, used multiple sensors, or used a biomechanical model based on a person’s height (an inverted pendulum model).
We leveraged previously collected data from an IMU (3D accelerometer) worn on the lower back to analyze a relatively large (472 subjects and more than 80,000 individual steps) and diverse set of data. The dataset included five different groups of participants with a range of health statuses and gait abilities: individuals with Parkinson’s disease (PD), people with mild cognitive impairment (MCI), individuals with multiple sclerosis (MS), healthy young adults, and older adults.
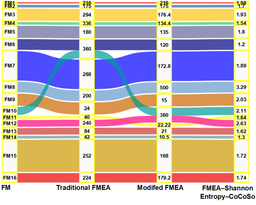
The collected 3-channel accelerometer data was represented by a set of computed features, which captured the temporal and spectral characteristics of each recorded step. Then, based on the derived feature set, we trained and tested several models, including XGBoost, logistic regression (LR), regression tree (RT), support vector machine (SVM), k-nearest neighbors (KNN), and an inverted pendulum, biomechanical model. Among these, the XGBoost provided the most accurate predictions, outperforming the state-of-the-art. The estimation error using the widely used biomechanical, inverted pendulum model was 20.6 cm; using the XGBoost model, the error was reduced to 6.08 cm (for a single step), as illustrated in Figure 1.
To further improve step length estimation (SLE) accuracy, we used an averaging technique that involved calculating the mean of estimated and measured step lengths across several consecutive steps. This method reduced the error (RMSE) from 6.08 cm to 5.21 cm, 4.98 cm, and 4.79 cm when averaging over 3, 5, and 10 steps, respectively.
Model generalizability was tested on validation datasets (distinct from the training of the model). While the error (RMSE) increased slightly for a distinct second validation set, the relative errors remained consistent. This result underscores the robustness of the model and its generalizability.
Overall, our results, tested in a relatively large and diverse group of subjects, show that the described XGBoost model can be used as an accurate step length estimator, even in older adults and people with relatively impaired gait due to aging or neurological disease. The relative simplicity of this method makes it a potential candidate for a single-device, wearable solution in clinical, controlled testing environments and perhaps also in real-world, uncontrolled settings.
More generally, our findings demonstrate how experts in different fields can work together to advance wearable sensor studies.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in