After the Paper | Human Intestine Chip: From Emulating Host-Microbiome Interactions to Disease Modeling and Therapeutic Development
Published in Bioengineering & Biotechnology

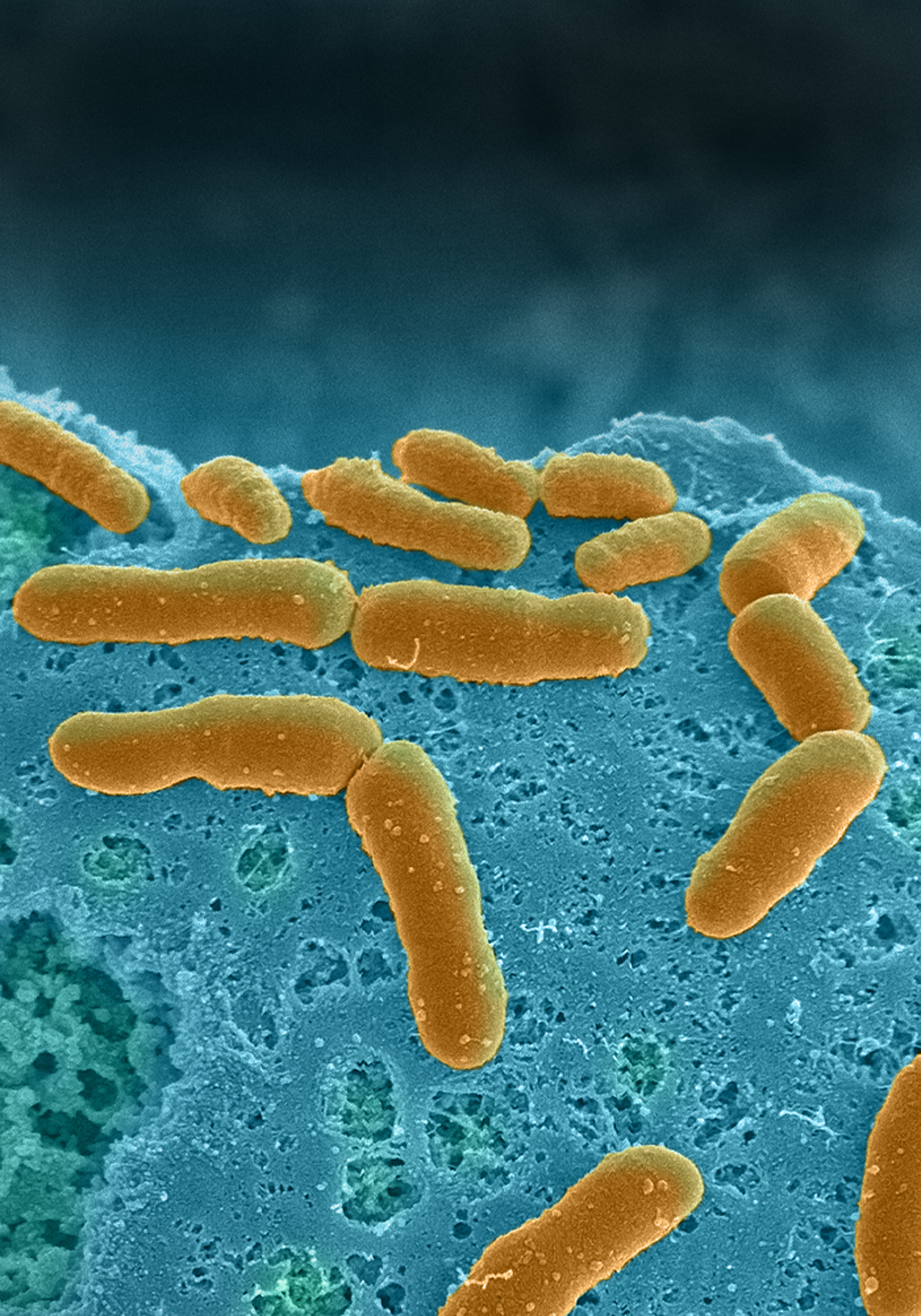
About a year ago, we published a paper in Nature Biomedical Engineering on the development of an anaerobic microfluidic model of human intestine (Intestine Chip) that enables the co-culture of highly complex human commensal microbiome with living, mucus-secreting human intestinal epithelium for extended times (Fig. 1). Thanks to an in vivo-like hypoxia gradient, both aerobic and anaerobic microbiota communities derived from human stool specimens survived and grew over time in human Intestine Chip. Our model accurately recapitulated in vivo behaviors, including the maintenance of an abundance of obligate anaerobic bacteria with ratios of Firmicutes and Bacteroidetes similar to those observed in human feces.
The Intestine Chip is one of the most advanced in vitro models providing new insight into host-microbiome interactions and microbial effects on drug safety and efficacy, and enables the development of microbiome-related diagnostics and therapeutics. Further, patient-derived intestinal cells and microbiome used in the Intestine Chip opens up opportunities for personalized medicine approaches. This platform supports the culture of region-specific intestinal tissue (e.g. duodenum, ileum and colon) and microbiomes from the same individual to find associations that cause sensitivity or tolerance to specific pathogenic, inflammatory, and systemic diseases.
Creating this on-chip physiologically relevant in vitro model was a fantastic opportunity to familiarize myself with different strains of bacteria and their role in human health and disease. Our study enabled investigation of host-microbiome interactions resulting in works recently published in Microbiome and CMGH journals. As one of the major publications of my PhD project, these findings strongly impacted my career transitioning my interests towards the microorganism–host crosstalk in my postdoctoral work. I am currently evaluating the interaction of the host immune system and mycobacterium tuberculosis, a species of pathogenic bacteria that affects millions of people every year.
Our paper ranked top three on Nature BME’s most visited articles of 2019 with over 11K unique views and gained a great deal of attention from academic institutes, industry sectors and funding agencies. In light of these results, I was awarded Lush Prize (UK), recognizing selected young researchers in the North America, and Ruth and William Silen Award (Harvard University, USA), and Ingber Lab managed to secure multiple grants/awards trough Bill & Melinda Gates Foundation, FDA, etc. This work opened multiple avenues of research that Ingber Lab is currently exploring, as well as offering new opportunities for collaborations. This methodology is being applied to other Organ Chip systems to model and study host−microbiome interactions in other organs (such as vagina, skin and lung).
While much more remains to be learned about real-time, dynamic and spatially resolved information of microorganism–microorganism and microorganism–host interactions, how microbial and host-cell viability changes over time or how their gene-expression profiles evolve during chip culture, our platform offers ample opportunities for the detailed study on direct and indirect host–microorganism crosstalk happens in the gut that would otherwise be challenging to answer in human and animal studies. This technology could be used to elucidate the mechanisms of human diseases, within and beyond the gastrointestinal system, and discover new therapeutics, probiotics and nutraceuticals.
Follow the Topic
-
Nature Biomedical Engineering

This journal aspires to become the most prominent publishing venue in biomedical engineering by bringing together the most important advances in the discipline, enhancing their visibility, and providing overviews of the state of the art in each field.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in