Association of in utero HIV exposure with child brain structure and language development: a South African birth cohort study
Published in General & Internal Medicine, Public Health, and Behavioural Sciences & Psychology

Introduction
Over 1 million children are born to mothers living with HIV every year, and in some countries, more than 1 in 5 children have HIV exposure. Thanks to antiretroviral medications there have been huge successes in preventing transmission of HIV, meaning that most of these children will remain HIV-free. However, although these children do not get HIV infection, being exposed to HIV in pregnancy may still increase the risk of poorer health, growth, and developmental outcomes. Evidence suggests more children with HIV exposure have delays in early language and motor function than children without HIV exposure. Brain development underpins cognitive function and advances in neuroimaging now allow us to study how HIV exposure may impact brain development. This research provides new insights into the potential effects of HIV exposure on child brain and language development.
What inspired this study and why is it important?
Early neurodevelopment is critical to later health and societal outcomes. Worldwide, over 250 million children under five are at-risk of not reaching their developmental potential, with the highest numbers in sub-Saharan Africa. The reasons for this are varied, and include factors like infectious diseases. Given many children in this region are exposed to HIV in pregnancy, it is crucial that we study how HIV exposure affects child brain development. Understanding the effects of HIV exposure on the brain may help guide interventions that ensure children not only remain HIV-free, but also thrive, reaching their full developmental potential.
What makes this study unique?
Neuroimaging of young children is extremely challenging because it requires them to stay still for long periods of time to capture high quality clear images. Across Africa there are also very few magnetic resonance imaging (MRI) scanners and access to imaging is therefore limited. This is the first study to examine the components of cortical brain structure in children with HIV exposure in pregnancy.
What did this study do?
The Drakenstein Child Health Study is a population-based birth cohort in the Western Cape of South Africa. In this study, we conducted MRI in natural sleep in children with HIV exposure and compared their brain structure to those without HIV exposure, and how it corresponded to language development outcomes.
What did the study show?
Children who were exposed to HIV in pregnancy showed differences in brain structure compared to children not exposed to HIV. Specifically, their brain cortex, particularly in the medial orbitofrontal region, was on average thicker than in children without HIV exposure. Secondly, children with HIV exposure had lower mean language scores compared to HIV-unexposed children, and the brain differences were linked to the lower language scores, Overall, the study found that differences in cortical brain structure in specific brain regions may partly explain the connection between HIV exposure and poor language outcomes.
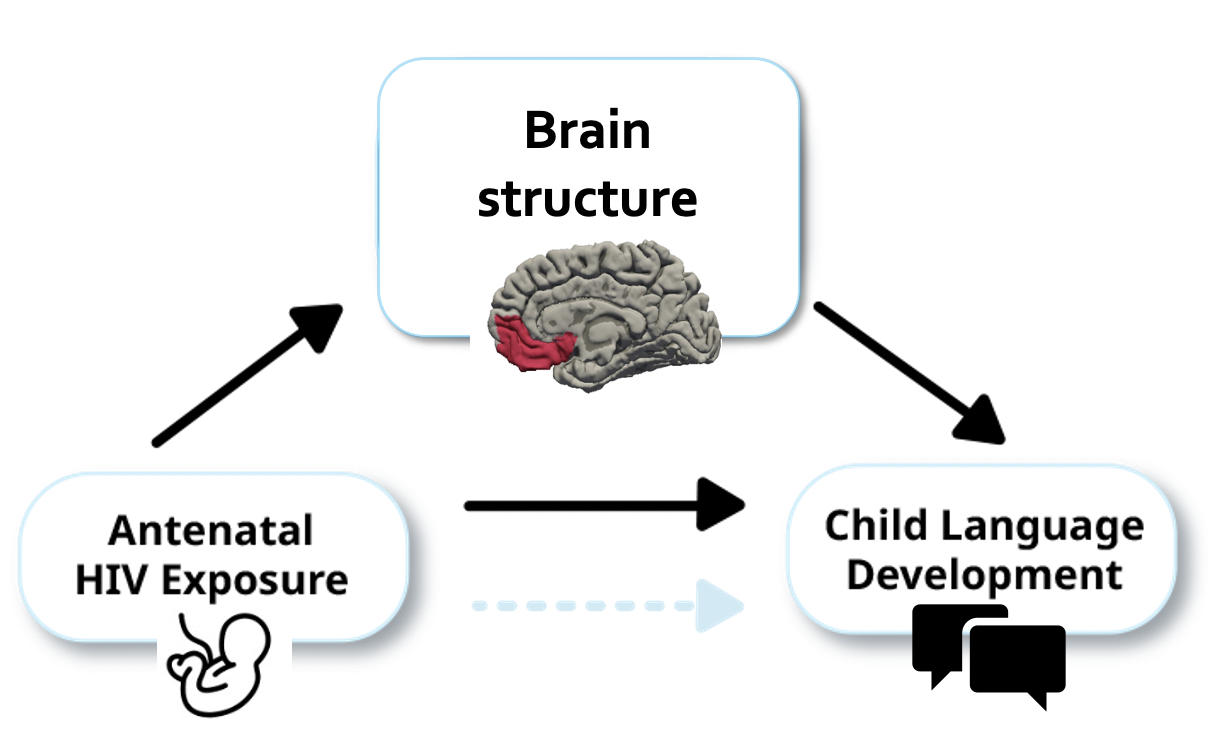
The main takeaway from this study is that HIV exposure in utero may impact early brain development and language function for some children. With over 16 million children worldwide who are HIV-exposed and uninfected, these findings may inform monitoring and intervention strategies to improve outcomes. Another recent study has shown that better maternal HIV care improves the child brain outcomes, which suggests ways to optimise neurodevelopment in the future. Finally, the study also highlights how brain development relates to language skills in all children.
References:
Gilmore JH, Knickmeyer RC, Gao W. Imaging structural and functional brain development in early childhood. Nat Rev Neurosci. 2018;19(3):123–37. DOI: 10.1038/nrn.2018.1
UNAIDS. AIDSinfo. Available from: http://aidsinfo.unaids.org
Wedderburn CJ, Subramoney S, Yeung S, Fouche JP, Joshi SH, Narr KL, et al. Neuroimaging young children and associations with neurocognitive development in a South African birth cohort study. Neuroimage. 2020;219:116846. DOI: 10.1016/j.neuroimage.2020.116846
Wedderburn CJ, Weldon E, Bertran-Cobo C, Rehman AM, Stein DJ, Gibb DM, et al. Early neurodevelopment of HIV-exposed uninfected children in the era of antiretroviral therapy: a systematic review and meta-analysis. Lancet Child Adolesc Health. 2022;6(6):393–408. DOI: 10.1016/S2352-4642(22)00071-2
Zar HJ, Barnett W, Myer L, Stein DJ, Nicol MP. Investigating the early-life determinants of illness in Africa: the Drakenstein Child Health Study. Thorax. 2015;70(6):592-4. DOI: 10.1136/thoraxjnl-2014-206242
Follow the Topic
-
BMC Medicine

This journal publishes outstanding and influential research in all areas of clinical practice, translational medicine, medical and health advances, public health, global health, policy, and general topics of interest to the biomedical and sociomedical professional communities.
Related Collections
With Collections, you can get published faster and increase your visibility.
Weight loss interventions and their health impacts
BMC Medicine is calling for submissions to our new Collection on weight loss interventions and their health impacts, emphasizing a variety of strategies, including dietary changes, physical activity, pharmacological treatments, and surgical options. We encourage submissions that explore the long-term effects of these interventions, adherence challenges, and strategies to address health inequities. The goal is to advance understanding and improve outcomes in weight management and overall health.
Weight loss interventions encompass a wide range of strategies aimed at reducing body weight and improving health outcomes. These interventions can include dietary changes, increased physical activity, pharmacological treatments, and surgical options such as bariatric surgery. As the global prevalence of obesity and related comorbidities continues to rise, understanding the efficacy and mechanisms of various weight loss interventions becomes increasingly crucial for public health. This Collection seeks to explore the diverse methodologies and outcomes associated with weight loss interventions, offering insights into their impacts on both individual and population health.
The significance of this research is underscored by the growing body of evidence linking obesity to numerous chronic health conditions, including diabetes, cardiovascular diseases, and certain types of cancer. Advances in pharmacological treatments, such as SGLT2 inhibitors and GLP-1 agonists, have emerged as promising options for weight management, demonstrating not only weight loss but also improved metabolic health. There are, however, challenges and limitations related to drug availability, healthcare delivery, and long-term treatment adherence with rapid weight gain when stopping treatment. Additionally, integrating behavioral strategies with nutritional and physical activity interventions has shown potential in enhancing adherence and long-term success. By further investigating these modalities, we can develop comprehensive approaches that address the multifactorial nature of obesity.
Continued research in this domain may yield innovative strategies that harness technology, such as mobile health applications and telehealth, to support weight loss interventions. As we deepen our understanding of the genetic, environmental, and behavioral factors influencing obesity, personalized interventions tailored to individual needs could emerge. This progress may lead to improved health outcomes, reduced health inequities, and ultimately a shift in the paradigm of obesity treatment and prevention.
We are looking for original manuscripts on topics including, but not limited to:
•Clinical trials investigating interventions for weight loss to promote health
•Real-world data on long-term effects and challenges of weight loss interventions
•Factors affecting long-term adherence to weight-loss or weight maintenance interventions
•Challenges and inequities in access to weight loss interventions
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being.
Publishing Model: Open Access
Deadline: May 07, 2026
Climate change and human health
BMC Medicine is calling for submissions to our new Collection on the health impacts of climate change. The relationship between global warming and human health is increasingly becoming a focal point in public health research. Rising temperatures, shifting weather patterns, and extreme weather events are projected to have profound effects on various health outcomes. From increased prevalence of vector-borne diseases to heightened risks of heat-related illnesses, the health implications of climate change are vast and multifaceted. This Collection aims to explore the direct and indirect impacts of global warming on health, examining how these changes affect vulnerable populations and health systems worldwide.
Understanding the implications of global warming for human health is crucial for developing effective public health strategies and interventions. Recent research has highlighted the links between climate change and a variety of health issues, including air pollution, water-borne diseases, and undernutrition. Advances in climate modeling and epidemiological studies have enhanced our ability to predict health outcomes related to climate change, providing invaluable insights that can inform policy decisions and health care planning.
Continued research in this area may lead to innovative solutions to mitigate the health impacts of climate change. For example, interdisciplinary approaches that integrate climate science, public health, and social determinants of health could reveal new pathways for adaptation and resilience. Future studies may also focus on the development of health infrastructure designed to withstand climate-related stresses, thus improving community health outcomes in an era of global warming.
We are considering manuscripts on, but not limited to the following topics:
-Impact of air pollution on health
-Heat-related illnesses
-Water-, and vector-borne diseases in a warming world
-Social determinants of health and climate vulnerability
-How health systems and infrastructure may be affected by climate change
-Nutrition and health in the context of climate change
-Impacts of climate change on non-communicable diseases
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 13 (Climate Action).
Publishing Model: Open Access
Deadline: Mar 02, 2026






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in