Behind the Paper: Introducing Computational Prophylaxis and the COHRCIE Framework
Published in Computational Sciences, Public Health, and Philosophy & Religion
Behind the Paper: Introducing Computational Prophylaxis and the COHRCIE Framework
What if disease prevention had its own computational science?
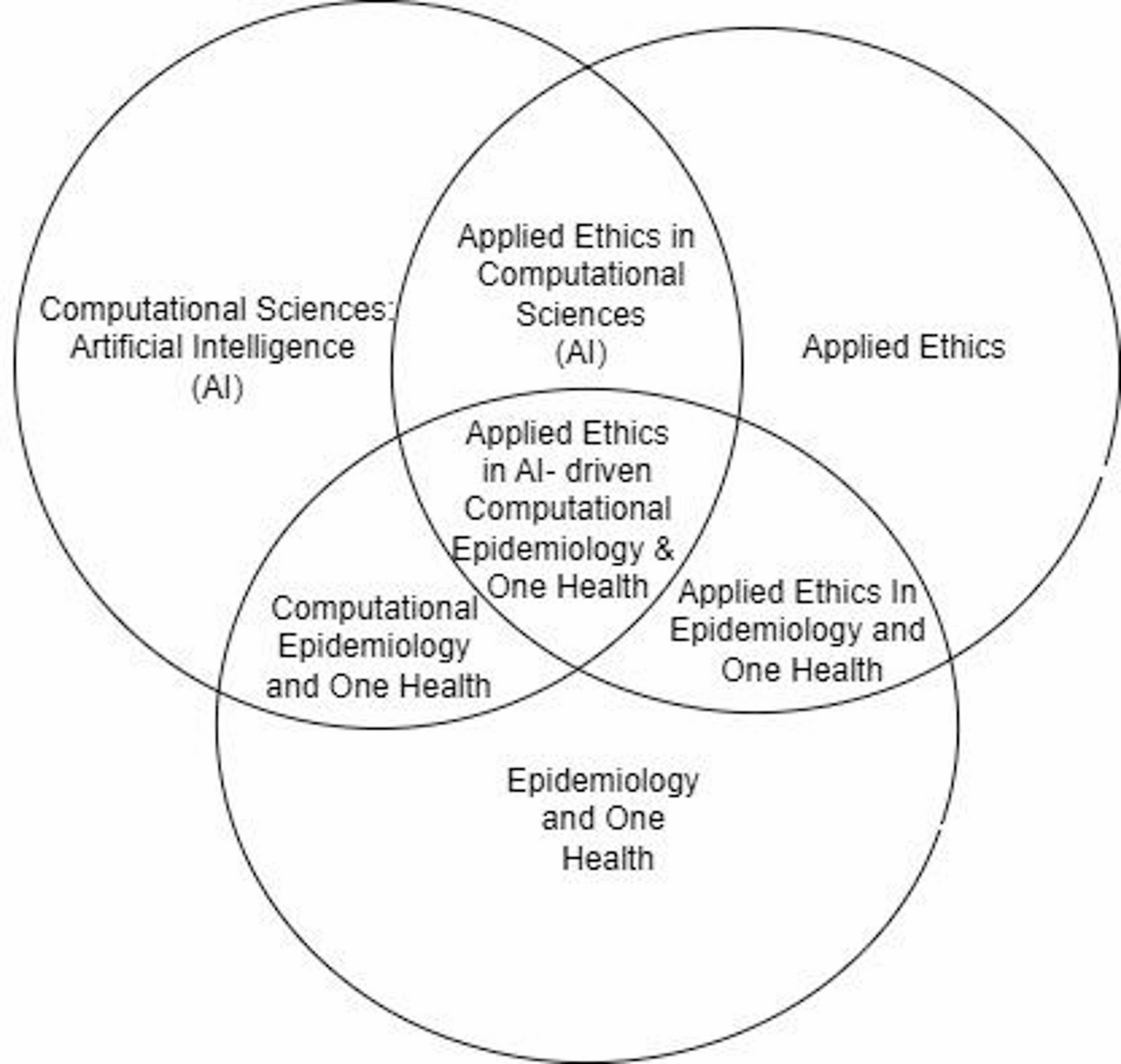
When I began my PhD research, I knew I wanted to work at the intersection of computer science, epidemiology, and the One Health paradigm. The need to situate my research within a clear field of study revealed a gap in the way we think about disease prevention. As a computer scientist working in epidemiology through the One Health paradigm, I realized that most computational approaches were framed around response: detecting, tracking, or predicting outbreaks once they had already begun. Very little attention was given to the prophylactic paradigm, the idea that computation could be used proactively, not just reactively, to stop outbreaks before they start.
My goal is to move beyond theoretical models and create real-world tools that prevent disease across environmental, animal, and human systems. It was this drive that led me to coin the term Computational Prophylaxis, and to develop the COHRCIE Framework as a way of grounding preventive computational methods in ethical responsibility.
The Spark Behind the Work
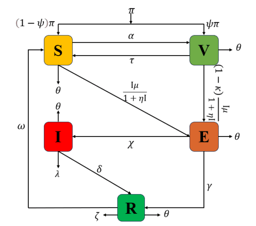
The COVID-19 pandemic made clear a reality that has always existed in public health. We are often several steps behind outbreaks. Computational models tend to be descriptive or predictive. They explain what happened, or they forecast what might happen. These are important, but they leave open a critical question: how do we design computational approaches that actively strengthen prevention before crises unfold?
As I reflected on this during the course of my doctoral studies, I saw the beginnings of an answer in the One Health paradigm. By linking human, animal, and environmental health, One Health provides a holistic view of disease emergence. The challenge was to bring computation and ethics into this paradigm in a way that actively supports prophylaxis.
Naming Computational Prophylaxis
The term Computational Prophylaxis was born from this gap. I wanted to create a language that signals a shift from computational epidemiology that reacts, to one that prevents. Naming a concept matters because it frames how others perceive and engage with it. For me, Computational Prophylaxis is about harnessing algorithms, simulations, and AI in ways that support proactive interventions, whether in pandemic preparedness, agricultural health, or environmental monitoring.
The COHRCIE Framework (Computational One Health Research Compliance and Integrated Ethics) complements this vision. It sets out principles for embedding ethics and responsibility into preventive computational work, ensuring that the pursuit of efficiency does not undermine equity, transparency, or trust.
Challenges Along the Way
Developing this paper was not without challenges. One of the most difficult aspects was balancing theoretical depth with clarity. At times, I wrote as though my audience were only computer scientists or only epidemiologists. Yet the strength of One Health lies in its interdisciplinarity. To communicate this vision, I had to reshape the narrative for a broader audience without losing academic rigor.
Another challenge was internal. The work required me to confront the limits of my own disciplinary training. As a computer scientist, I am comfortable with algorithms, models, and technical systems. But placing these in the context of ethics and public health policy pushed me into less familiar territory. In hindsight, that stretch was essential. It shaped the interdisciplinary voice that this paper now carries.
Why Ethics and One Health Matter
Artificial intelligence is increasingly applied in health research and practice. From disease surveillance to drug discovery, algorithms are shaping decisions that affect millions of lives. Yet algorithms do not operate in a vacuum. They reflect the values, priorities, and limitations of those who design and deploy them.
This is why ethical grounding is not optional. In One Health, the consequences of neglecting ethics are magnified. A model that prioritizes human outcomes without considering animal or environmental spillovers may inadvertently worsen future risks. By embedding ethics directly into the framework of Computational Prophylaxis, the COHRCIE approach helps guard against such blind spots.
Looking Ahead
I see this paper as the beginning of a conversation, not the final word. Computational Prophylaxis is a starting point for a larger research agenda. In practical terms, it can influence pandemic preparedness by guiding where resources are allocated before outbreaks. It can support agriculture by modelling and preventing zoonotic diseases that originate in livestock. It can help environmental health by identifying conditions that increase disease emergence in ecosystems.
The COHRCIE Framework provides a roadmap for researchers, policymakers, and technologists who want to ensure that these efforts remain ethically sound and socially responsible.
Personal Reflections
For me, publishing this article represents a moment of crystallization in my PhD journey. The work reflects years of thinking, refining, and sometimes struggling to articulate what I felt was missing in the literature. Seeing the concept of Computational Prophylaxis formally enter scholarly discourse is deeply affirming.
At the same time, I recognize that this is only the first step. Ideas gain life when they are engaged with, critiqued, and built upon by others. I am hopeful that this article will invite collaboration and provoke dialogue across disciplines.
Closing Thoughts
My vision for Computational Prophylaxis is not just academic. It is about shaping tools and approaches that can prevent suffering in human, animal, and environmental populations. It is about strengthening the ethical spine of computational epidemiology so that future systems serve not just efficiency, but equity and responsibility.
I invite fellow researchers, practitioners, and students to explore this idea, challenge it, and expand it. If you are interested in shaping the future of Computational Prophylaxis and ethical AI in One Health, I welcome the opportunity to connect.
Follow the Topic
-
Discover Public Health

This is an open access journal publishing research from all fields relevant to public health.
Related Collections
With Collections, you can get published faster and increase your visibility.
Antimicrobial Resistance: The New Challenge to Global Health in a Post-Pandemic World
Antimicrobial resistance (AMR) is a seriously ongoing threat to global health, occurring when bacteria, fungi, viruses, and parasites evolve to resist the drugs designed to kill or block them. The COVID-19 pandemic has both directly and indirectly exacerbated the problem of AMR, as the overuse of antibiotics has accelerated the development of resistance in many pathogens. COVID-19 may have subsided, but AMR continues to pose a significant risk to the effectiveness of global healthcare systems, threatening to reverse decades of progress in combating infectious diseases. The interplay between population health and AMR has become increasingly critical as healthcare practices have shifted in response to the pandemic. Understanding this relationship is essential for developing effective strategies to mitigate the impact of AMR on population health in a post-COVID context.
The motivation for launching this Collection arises from the urgent need to address the rising tide of AMR as healthcare systems grapple with the long-term effects of the pandemic. Increased antibiotic use during COVID-19 treatment, changes in healthcare access, and disruptions in public health interventions have all contributed to an environment where AMR can thrive. Moreover, the pandemic has highlighted the importance of a multidisciplinary approach to tackling AMR, involving epidemiology, policymaking, and community health initiatives. This Collection aims to provide a platform for researchers and practitioners to share insights and findings that can inform future strategies to combat AMR while considering the broader implications for population health.
This Collection aims to highlight the multifaceted nature of AMR in a post-pandemic environment. We solicit articles that investigate the particular issues provided by the pandemic in terms of AMR development and containment, examine the impact of AMR on many sectors of healthcare, and propose novel strategies to minimize resistance propagation. Submissions may include original research, policy assessments, program evaluations, and comments on the following major areas:
• Epidemiology and trends of AMR post-pandemic
• Impact of COVID-19 on antibiotic usage
• Surveillance strategies for AMR
• AMR and stewardship
• Prevention and control measures to limit AMR spread
• Policies and programs to promote antibiotic stewardship
• Economic and social implications of AMR
• Global collaboration and initiatives to tackle AMR
By addressing these critical issues, this Collection aims to provide a comprehensive understanding of the emerging challenges in antimicrobial resistance in a post-pandemic world and to promote effective strategies to preserve the power of our current antimicrobials.
Keywords: antimicrobial resistance; COVID-19; antibiotics; global health; infectious diseases; public health; policy; prevention
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Jun 30, 2026
Health Literacy and Informal Caregiving
Personal and health service literacy limitations are significant predictors of poor healthcare access, suboptimal health behaviors (e.g., physical inactivity, smoking), and adverse outcomes, leading to increased emergency visits, hospitalizations, and premature mortality—particularly among informal caregivers and their care recipients. Informal caregivers, especially in low- and middle-income countries (LMICs), often make critical health and healthcare decisions that impact both their own outcomes and those of the individuals they care for. Therefore, interventions aimed at enhancing health literacy among informal caregivers are essential for improving health outcomes, healthcare utilization, and lifestyles. We invite submissions addressing, but not limited to, the following topics:
We invite submissions addressing, but not limited to:
1. Health literacy assessments of informal caregivers
2. Sociocultural determinants of caregiver health literacy
3. The impact of health literacy on caregiver burden, health status, and outcomes
4. Interventions to promote health literacy among informal caregivers
Submissions from low- and middle-income countries are highly encouraged, while studies from high-income countries will also be considered based on their novelty, robustness, and strength of evidence.
This Collection supports and amplifies research related to SDG3 and SDG10.
Keywords: Health literacy; informal caregiving; wellbeing; quality of life; health equity
Publishing Model: Open Access
Deadline: Feb 28, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in