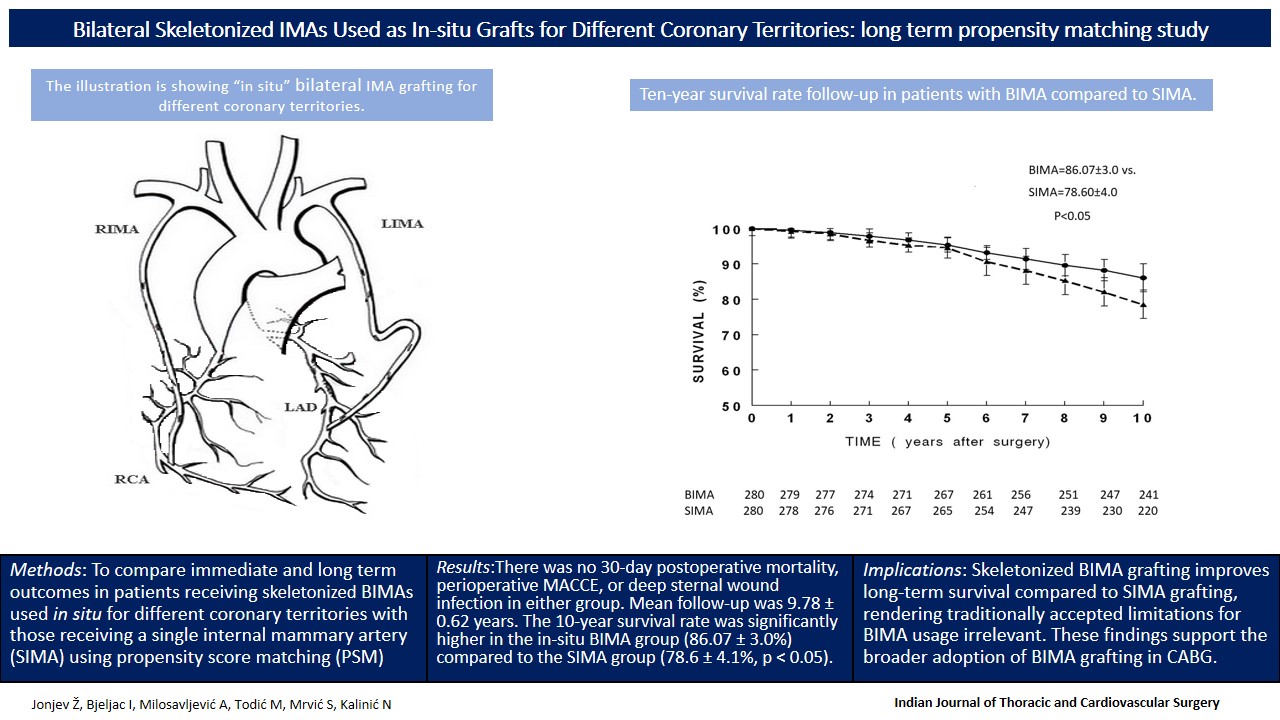
Bilateral skeletonized IMAs used as “in situ” grafts for different coronary territories: long-term propensity matching study
Published in Biomedical Research and Surgery

1. What motivated this research?
Despite decades of evidence supporting the use of bilateral internal mammary arteries (BIMAs) in coronary artery bypass grafting (CABG), their adoption remains disappointingly low in routine practice. Concerns about technical complexity, sternal wound complications, and patient comorbidities continue to discourage many surgeons from utilizing this superior revascularization strategy.
As a cardiac surgeon with over three decades of experience, I’ve consistently witnessed the long-term benefits of arterial grafting. However, there remained a critical gap in real-world, long-term data evaluating the safety and efficacy of skeletonized, in-situ BIMA grafting in everyday practice.
2. What’s new or different in your study?
This study is one of the few to report nearly 10-year outcomes of skeletonized in-situ BIMA grafting using propensity-matched controls. We demonstrated a clear long-term survival advantage over conventional SIMA grafting with zero perioperative mortality or sternal wound complications.
3. What were the main challenges?
The main challenge was surgical consistency—ensuring a standardized skeletonization technique and avoiding confounding factors over a 10-year period. Another was assembling a well-matched control group for meaningful comparison, which required rigorous data validation.
This study emerged from a simple but pressing question: Are the traditional concerns about BIMA grafting still valid today?
4. What surprised you the most?
To our surprise—and satisfaction—the BIMA group demonstrated superior long-term survival, zero perioperative mortality, and no deep sternal wound infections, challenging outdated limitations. These results underscore the importance of surgical technique, careful patient selection, and institutional experience in achieving excellent outcomes.
5. Why does this matter for patients or practice?
Our results suggest that BIMA grafting should no longer be reserved for a select few. With careful technique and experience, it’s not only feasible—it significantly improves survival.
6. Final personal reflection or message to peers
Through this research, we aim to shift the mindset from "BIMA is risky" to "BIMA is standard—when done right." We hope this encourages broader use of this technique, ultimately improving long-term results for patients undergoing CABG.
Follow the Topic
-
Indian Journal of Thoracic and Cardiovascular Surgery

The Indian Journal of Thoracic and Cardiovascular Surgery is a double-blind peer review journal focusing on current clinical practices and developments in cardiovascular surgery.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in