Biological rhythms and sleep in head-down tilt bed rest conditions: insights from a long duration protocol in men
Published in Astronomy and Anatomy & Physiology

Space flight and spending two months constantly in bed might seem like two completely different situations. However, constant bed rest is a protocol that both the European Space Agency and the National Aeronautics and Space Administration (NASA) frequently use to simulate the effects of microgravity on the human body. With a twist: bed rest must involve lying with the head at a slightly lower level than the rest of the body.
Head-down tilt bed rest simulates the effects that space travel, with its corresponding reduction in gravitational force, can have on our bodies. Among these physiological changes are the loss of muscle and bone mass, alterations in the cardiovascular system, or disruptions in metabolic, immune, and cognitive processes. However, a less-studied aspect of physiology concerning the effects of microgravity is sleep and biological rhythms.
Circadian physiology
Our physiological processes exhibit variations throughout the day that repeat with a period of around 24 hours. These circadian (about a day) rhythms arise thanks to a hierarchical system of structures directed by a central pacemaker, the suprachiasmatic nucleus, located in the hypothalamus. This central clock, which has a slightly longer than 24-hour period, adjusts and resets daily due to different inputs or temporal signals, with the light-dark cycle being the fundamental one. Additionally, this system has several outputs, which are precisely the rhythms we can measure. Among them are the sleep-wake cycle, periodic postural changes, secretion of most hormones, rhythms in body temperature and in motor activity. Importantly, these outputs can also influence, via feedback, the functioning of the clock itself and exposure to inputs.
In space travel, besides microgravity, other factors like changes in the light-dark cycle contribute to the disruption of the circadian system and the sleep-wake cycle. However, a head-down tilt bed rest protocol permits us to isolate the potential effect of microgravity on these processes. Furthermore, this protocol is also interesting from a circadian perspective as it allows the dissociation of the postural cycle of standing-laying (absent in space) from the sleep-wake cycle, which would be linked under normal free life conditions.
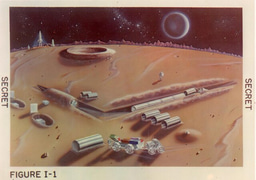
This was the protocol implemented by the European Space Agency at the MEDES Space Clinic in Toulouse throughout 2017. Twenty men were selected to embark on the adventure of spending 3 months confined to the clinic, with 2 of those months spent constantly lying down with their heads tilted down at a 6-degree angle. They conducted all their daily activities in this position, from eating to all imaginable physiological needs, including personal hygiene tasks.
Sleeping (and living) in head down position for 60 days
Sixteen international groups took part in the study, focusing on evaluating different aspects of the physiology of these volunteers undergoing this microgravity simulation. The Sleep Group from the University of Surrey, led by Simon N. Archer, focused on studying sleep and other biological rhythms in this group of volunteers. For this purpose, we equipped them with wrist-worn devices that allowed us to track the evolution of their peripheral temperature rhythms, motor activity, and exposure to light over those three months. They also completed a daytime sleepiness questionnaire four times a day, and through electroencephalogram, we objectively evaluated their sleep during the day and night in several sessions throughout the study. During those sessions, we also collected saliva samples that allowed us to determine the phase and amplitude of hormone secretion rhythms such as melatonin and cortisol.
The results we obtained were clear: although the light-dark cycle remained somewhat normal (considering the study was conducted indoors), the amplitude of temperature, activity, and daytime sleepiness rhythms clearly decreased during the bed rest phase compared to the baseline and recovery segments. However, the phase (i.e., time of day those rhythms occurred) remained unchanged regarding melatonin and cortisol secretion (with some alterations in their concentrations), probably due to the maintenance of the light-dark cycle.
Participants slept less than 6.5 hours during the night, tending to decrease this duration upon entering the bed rest phase and lengthening it throughout this segment of the study. During the day, however, the trend was opposite: upon starting bed rest, daytime sleep increased by almost 15 minutes compared to the previous segment.
An important finding of this study has also been to verify that peripheral skin temperature at the wrist shows a clear temporal association with melatonin secretion, especially in the morning, during the descending phase, even under bed rest conditions. The change in peripheral temperature associated with different sleep stages (wrist skin temperature increases as sleep becomes deeper), however, was lost during the bed rest phase, which could also indicate a disruption in thermoregulation processes related to sleep.
This is the first time that sleep and various biological rhythms have been evaluated from an integrative perspective in a head-down tilt bed rest protocol of this long duration (60 days). We are confident that these findings will serve in designing new protocols aimed at improving sleep and rhythmic robustness in space.
Dr. María-Ángeles Bonmatí-Carrión & Prof. Simon Archer
(Picture by Kobby Mendez in Unsplash)
Follow the Topic
-
npj Microgravity

This journal aims to provide a thorough understanding of the scientific impact and future of spaceflight research.
Related Collections
With Collections, you can get published faster and increase your visibility.
Space Biomanufacturing
Publishing Model: Open Access
Deadline: Mar 15, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in