Breast Cancer Awareness Month: Highlights of breast cancer research from the BMC Series
Published in General & Internal Medicine and Surgery

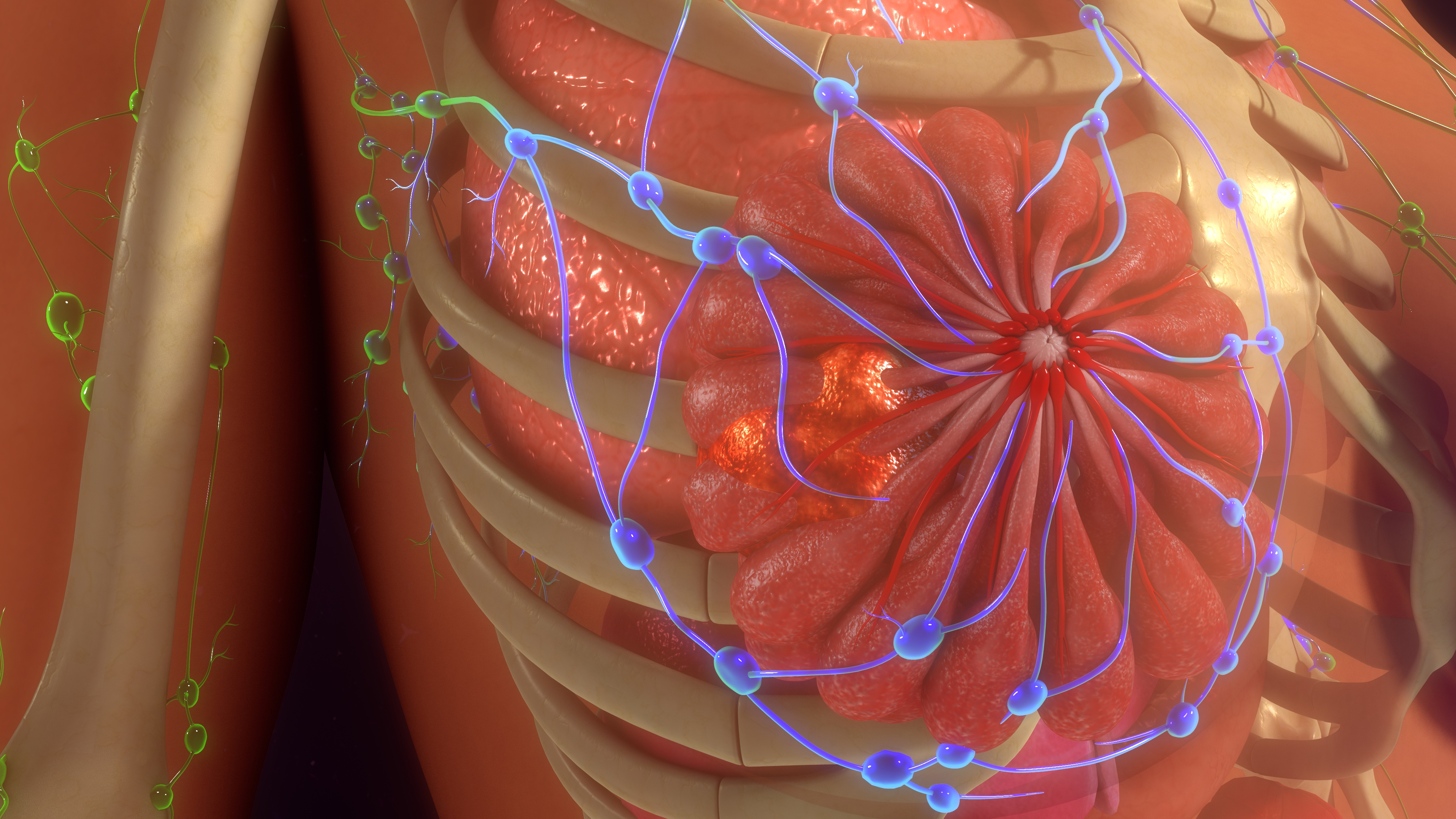
Breast cancer is a multifaceted disease that affects millions of individuals worldwide and stands as one of the leading causes of cancer-related mortality among women. Beyond the physical toll, its impact extends to emotional, social, and economic dimensions — disrupting daily life, straining relationships, and challenging access to care. Symptoms and experiences vary widely, from lumps and fatigue to the psychological burden of diagnosis and treatment.
Despite its global prevalence, breast cancer remains under-recognized in many communities, under-diagnosed due to limited screening access, and under-treated in low-resource settings. Addressing these gaps requires more than awareness — it demands action rooted in science, equity, and compassion.
Can a rare inflammatory breast disease mimic cancer even after mastectomy?
BMC Women’s Health - Recurrent Granulomatous Mastitis in the Contralateral Breast Following Radical Mastectomy for Breast Cancer
Granulomatous Mastitis (GM) is characterized by chronic inflammation, painful breast masses, and skin changes. Its etiology remains unclear, and it lacks specific imaging markers, which often leads to misdiagnosis or unnecessary interventions.
This case report, published in BMC Women's Health, details a rare and complex presentation of recurrent granulomatous mastitis (GM) in a 31-year-old woman who had previously undergone a radical mastectomy for triple-negative breast cancer in her right breast. Three years post-surgery, she developed GM in her left breast, a condition that is benign but often clinically resembles breast cancer, making diagnosis particularly challenging. Diagnosis was ultimately confirmed through histopathological analysis, ruling out cancer recurrence.

The literature review accompanying the case emphasizes that GM is most common in young women of childbearing age, and while it is non-cancerous, its presentation can be alarming. The authors note that GM can occur even in the contralateral breast post-mastectomy, which is exceptionally rare and not well-documented.
The study concludes that greater clinical awareness is essential to distinguish GM from malignancy, especially in patients with a history of breast cancer. It advocates for biopsy-based confirmation and cautions against relying solely on imaging. The case underscores the importance of a multidisciplinary approach involving radiologists, pathologists, and oncologists to avoid overtreatment and ensure accurate diagnosis.
This report contributes to the growing body of evidence that not all post-mastectomy breast masses are malignant, and highlights the need for more research into GM’s pathogenesis and management strategies.
Can a web-based tool help breast cancer patients make better decisions about reconstruction?
BMC Women’s Health - Effects of a Web-Based Decision Aid on Breast Cancer Patients Considering Breast Reconstruction
This randomized controlled trial, published in BMC Women’s Health, evaluated the impact of a web-based decision aid (WDA) on breast cancer patients facing choices about breast reconstruction surgery. The study involved 70 participants in China, randomly assigned to either a WDA group or a control group receiving standard paper-based information. The WDA included interactive modules for decision assessment, support, and evaluation, accessible via mobile devices at any time.
The findings revealed that patients using the WDA experienced greater decision-making confidence, lower decisional conflict, and higher satisfaction with their choices compared to those in the control group. The tool helped patients better understand their surgical options, risks, and outcomes, enabling more informed and personalized decisions. Importantly, the WDA also facilitated shared decision-making between patients and healthcare providers, aligning with modern patient-centered care practices.

The study concluded that digital tools like WDAs can play a crucial role in supporting breast cancer patients, especially when navigating complex treatment pathways. Given the emotional and physical implications of breast reconstruction, providing accessible, evidence-based decision support is essential. The authors recommend broader implementation of such tools in clinical settings to enhance patient autonomy and improve the quality of care.
This research underscores the growing importance of technology in healthcare communication, particularly in oncology, where treatment decisions are deeply personal and often overwhelming. As digital literacy increases globally, web-based aids offer a scalable, cost-effective solution to empower patients and reduce decisional stress.
What drives young women in Ethiopia to self-screen for breast cancer?
BMC Women’s Health - Self-Screening Practice of Breast Cancer Among Female Students in Ethiopian Universities
A 2024 cross-sectional study published in BMC Women's Health investigated the self-screening practices of breast cancer among female students in Ethiopian universities using the Theory of Planned Behavior (TPB). Breast cancer remains the most common cancer among women globally, and early detection through breast self-examination (BSE) is a critical preventive strategy—especially in low-resource settings like Ethiopia.

The study surveyed over 400 female students across multiple universities to assess their knowledge, attitudes, perceived behavioral control, and intentions related to BSE. Despite high awareness of breast cancer, only 20.6% of participants reported practicing regular self-examinations. The findings revealed that positive attitudes, strong intentions, and perceived control over the behavior were significantly associated with actual self-screening practices. Conversely, lack of confidence, limited access to information, and cultural taboos were major barriers.
The study concluded that while awareness campaigns have reached many students, behavioral change remains limited without structured support. The TPB framework proved effective in identifying psychological and social factors influencing BSE behavior. Researchers recommend integrating breast cancer education into university health programs and leveraging peer-led initiatives to normalize self-screening.Importantly, the study calls for policy-level interventions to promote early detection strategies among young women, aligning with global health goals such as SDG 3.4, which targets reducing premature mortality from noncommunicable diseases. By addressing both knowledge gaps and behavioral barriers, Ethiopia can improve early diagnosis rates and reduce breast cancer-related deaths.
Could your microbiome hold clues to breast cancer risk and treatment?
BMC Women’s Health - Breast Cancer and Microbiome: A Systematic Review Highlighting Challenges for Clinical Translation
This study explored the emerging relationship between breast cancer and the human microbiome, aiming to identify microbial signatures associated with cancer development, subtypes, and outcomes. The authors analyzed studies from databases including PubMed, Embase, Scopus, and Web of Science, focusing on bacterial genera found in breast tissue, gut, and other body sites of breast cancer patients.
The review found that certain bacterial genera—such as Escherichia, Staphylococcus, and Bacillus—were more prevalent in breast cancer tissues, while others like Lactobacillus appeared protective. These microbial patterns varied across cancer subtypes and stages, suggesting potential roles in tumor progression, immune modulation, and treatment response. However, the authors caution that methodological inconsistencies, such as differences in sample collection, sequencing techniques, and data analysis, limit the reproducibility and comparability of results.
Despite the growing interest in microbiome-based diagnostics and therapies, the review emphasizes that clinical translation remains premature. Most studies are observational, and few establish causality or offer standardized protocols. The authors call for larger, longitudinal studies with harmonized methodologies to validate findings and explore therapeutic applications like probiotics, antibiotics, or microbiome-targeted drugs.
In conclusion, while the microbiome presents a promising frontier in breast cancer research, significant scientific and logistical barriers must be overcome before it can inform routine clinical care. The review advocates for interdisciplinary collaboration and investment in microbiome science to unlock its full potential in cancer prevention, diagnosis, and treatment.
How does stigma around breast cancer affect future doctors in Egypt?
BMC Public Health- Exploring Breast Cancer Stigma Among Medical Students in Egypt
A 2025 national multi-center cross-sectional study published in BMC Public Health examined the prevalence and nature of breast cancer-related stigma among medical students in Egypt. Despite their future roles as healthcare providers, many students held stigmatizing beliefs that could negatively impact patient care and early diagnosis efforts.
The study surveyed over 1,000 students from multiple medical schools across Egypt, using a validated stigma assessment tool. Findings showed that a significant proportion of students associated breast cancer with shame, fear, and social isolation. Female students reported slightly lower stigma levels than males, and students in clinical years were generally more informed and less judgmental than those in preclinical years. However, misconceptions—such as breast cancer being contagious or caused by personal behavior—were still present.
Cultural norms and lack of open discussion about women’s health were identified as key contributors to stigma. The study also found that students who had personal or family experience with breast cancer were more empathetic and less likely to stigmatize the disease.

The authors concluded that medical education in Egypt needs to address breast cancer stigma more directly, integrating psychosocial and cultural dimensions into the curriculum. They recommend targeted awareness campaigns, patient interaction opportunities, and training in empathetic communication to prepare students for real-world clinical settings.
This research highlights a critical gap in healthcare training: knowledge alone isn’t enough—attitudes matter. Reducing stigma among future doctors is essential for improving breast cancer outcomes, especially in societies where cultural taboos hinder early detection and treatment.
Follow the Topic
-
BMC Public Health

An open access, peer-reviewed journal that considers articles on the epidemiology of disease and the understanding of all aspects of public health.
-
BMC Women's Health

This is an open access, peer-reviewed journal that considers articles on all aspects of the health and wellbeing of adolescent girls and women, with a particular focus on the physical, mental, and emotional health of women in developed and developing nations.
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Cancer in older adolescents and young adults
BMC Public Health is calling for submissions to our Collection on Cancer in older adolescents and young adults.
Cancer in older adolescents and young adults presents unique epidemiological challenges, with distinct patterns of incidence, risk factors and outcomes compared to other age groups. This Collection aims to enhance our understanding of cancers that affect these populations, such as gastrointestinal, endometrial, colorectal, cervical and breast cancers, some of which are HPV- or obesity-related. We invite research that explores disparities in cancer outcomes and advances evidence-based strategies for prevention, early detection, and management. For the purposes of this collection, we define older adolescents and young adults as being between 15 to 39 years old.
Topics of interest related to cancer in older adolescents and young adults include but are not limited to:
• Recent and longer-term trends in the incidence and mortality of different types of cancer
• Role of infectious, environmental, and lifestyle factors in cancer development
• Impact of obesity at age of diagnosis or prior obesity (such as during childhood) on subsequent cancer risk and outcomes
• Disparities in outcomes by race, ethnicity, and socioeconomic status
• Innovations in cancer prevention, screening, and early detection
• Long-term survivorship and quality of life among cancer survivors
• Policy implications for cancer prevention and control in younger populations
This collection supports and amplifies research related to SDG 3 Good Health & Well-Being.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 26, 2026
Endocrine disruption as a public health issue
BMC Public Health invites submissions to our new Collection, Endocrine disruption as a public health issue. Endocrine disruption has emerged as a growing public health challenge, characterized by the interference of certain chemicals with the normal functioning of the endocrine system. Endocrine disrupting chemicals (EDCs) can mimic, block, or alter hormone signaling, leading to a range of adverse health outcomes. Common sources of EDC exposure include everyday products such as plastics, pesticides, and personal care items, all of which can release substances like bisphenols and phthalates into the environment and human body. Understanding the links between exposure to EDCs and eventual health outcomes is vital for assessing their implications for population health.
We welcome submissions that delve into various aspects of endocrine disruption. Key topics of interest include, but are not limited to:
Role of EDCs in metabolic, endocrine and immune-related disorders
Effect of EDCs in consumer products including personal care products
The links between EDC exposure and male and female reproductive health problems
The links between EDC exposure and certain cancers
Insights into the long-term consequences of early-life EDC exposure and transgenerational effects
Methodological advances in assessing the health impacts of EDC mixtures and cumulative exposures
Development and application of statistical approaches to better estimate the health effects of chronic and/or concurrent exposure
Validating models of cumulative exposure with measurement of combinations of EDCs in human tissues
Individual- and policy-level interventions to address health impacts of EDC exposures
The search for substitutes lacking endocrine disrupting properties
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: May 26, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in