Closing the Gaps in Long-Term Breast Cancer Care: A Systematic Review of Clinical Practice Guidelines
Published in Healthcare & Nursing, Cancer, and General & Internal Medicine

The story behind our paper:
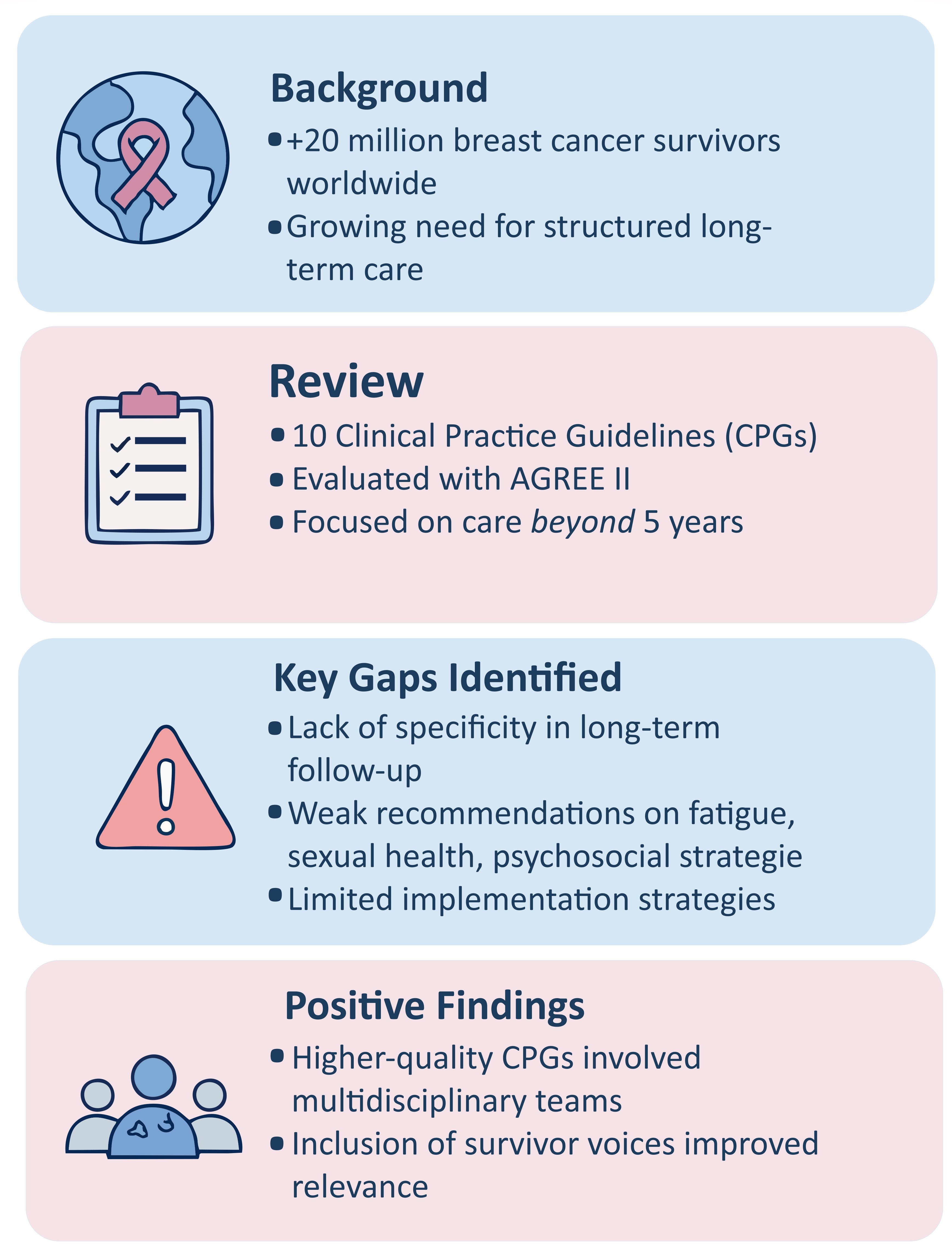
Breast cancer survivorship has changed dramatically in recent decades. Thanks to advances in early detection and treatment, the number of women living years—and even decades—after a breast cancer diagnosis continues to grow. But surviving is not the same as living well. Many women face persistent challenges after treatment ends: fatigue, pain, emotional distress, fear of recurrence, and difficulties navigating follow-up care.
Despite these needs, clinical practice guidelines (CPGs) often focus primarily on the acute phase of cancer treatment. Survivorship care, especially beyond the first five years after the completion of primary treatment, remains inconsistently addressed in many health systems. This was the motivation behind our systematic review: to examine the extent to which existing CPGs support the long-term health and well-being of breast cancer survivors.
As a health researcher working in the field of cancer survivorship, I wanted to understand whether the guidance we offer professionals truly reflects the needs of the growing population of long-term survivors.
Why guidelines matter:
Clinical practice guidelines shape decisions in clinics, hospitals, and health systems. When they are methodologically sound and inclusive, they offer essential support for quality care. But if they are outdated, vague, or lacking evidence, they risk leaving survivors with unmet needs.
In this review, we evaluated the methodological quality of current guidelines using the AGREE II instrument and analyzed the scope and content of their recommendations related specifically to long-term breast cancer survivorship. We focused on areas such as follow-up care, management of late and long-term effects, lifestyle interventions, and psychosocial support.
What we found:
We included 10 clinical practice guidelines published over the past decade. While some offered useful recommendations for survivorship care, many lacked specificity regarding the long-term phase, particularly beyond five years after the end of primary treatment.
Key issues such as fatigue, sexual health, return to work, or fear of recurrence were either insufficiently addressed or discussed in broad terms. Implementation strategies were often absent, and in many cases, the evidence base behind recommendations was unclear or poorly reported.
However, we also identified positive trends. Guidelines that had engaged multidisciplinary teams and included input from survivors themselves tended to demonstrate higher methodological quality. This highlights the importance of collaborative, patient-centered approaches in guideline development.
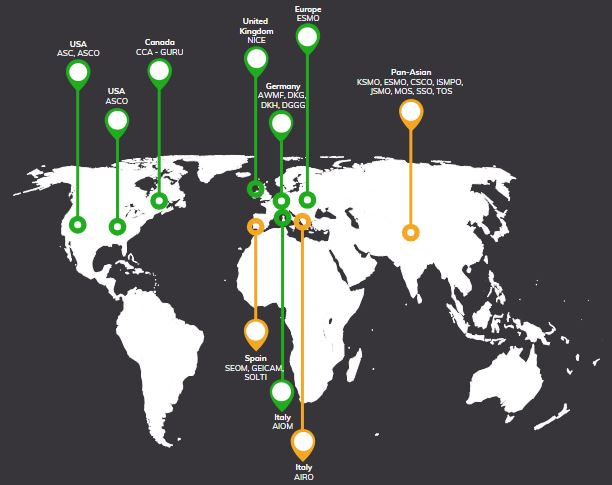
Global Distribution, Quality, and Developers of Breast Cancer Survivorship Guidelines.
Based on AGREE II scores: Green: High-quality | Amber: Moderate-quality
Challenges and reflections:
One of the biggest challenges was the inconsistent use of terminology. “Long-term survivorship” is not uniformly defined across guidelines, making both clinical practice and evidence synthesis more complex.
We also observed limited attention to equity-related issues. Few guidelines provided tailored recommendations for populations such as older survivors, minorities, or individuals in low-resource settings—groups who often face unique barriers to post-treatment care.
This raised an important question for us: Are we truly designing care pathways that serve all survivors, or only a subset?
Gaps in Long-Term Breast Cancer Survivorship Guidelines
Why this matters now:
As survivorship becomes an increasingly prominent phase in the cancer care continuum, we must ensure that our clinical guidance evolves accordingly. Survivors need and deserve care that is personalized, proactive, and grounded in robust evidence.
We hope that our review encourages clinicians, researchers, and policy-makers to re-examine how survivorship care is addressed in current guidelines—and to advocate for a broader, more inclusive perspective.
Final thoughts:
This work reflects a broader concern: that the voices and experiences of long-term breast cancer survivors are not yet fully reflected in clinical recommendations. Our findings call attention to gaps that must be closed if we are to deliver truly comprehensive care.
For me, this project reinforced the idea that survivorship is not an afterthought. It is a vital, complex phase of life that deserves the same level of attention, rigor, and compassion as diagnosis and treatment.
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in