Contact tracing in New York City
Published in Healthcare & Nursing
Contact tracing is an important tool for infectious disease control. During the COVID-19 pandemic, many locations implemented contact tracing to reduce the transmission of SARS-CoV-2. In New York City (NYC), the NYC Test & Trace Corps initiative (T2) was launched in June 2020. Established as an operation to provide contact tracing, testing, and resources to support isolation and quarantine, the contact tracing program was integrated with a set of intervention efforts designed to limit morbidity and mortality from COVID-19 in NYC.
One of the pressing questions during the pandemic is how to use the data collected through contact tracing to support decision-making. In October 2020, we established collaborations with T2 and the New York City Department of Health and Mental Hygiene (DOHMH), who provided us detailed contact tracing data and testing results within NYC. In this study, we analyzed contact tracing records for 644,029 cases and their contacts in New York City during the second pandemic wave between October 1, 2020 and May 10, 2021.
The initial goal of the analysis was to establish transmission chains at the individual level. It was not long before we realized that this goal was unrealistic as self-reported close contacts were predominately household members (over 90%). With such a high level of bias, it is unlikely complete transmission chains can be meaningfully reconstructed. We therefore shifted our goals to address the three following questions:
(1) What was the operational performance of contact tracing?
(2) How did SARS-CoV-2 spread across NYC communities?
(3) What were the effects of control measures and vaccination on the spatial expansion of SARS-CoV-2 in NYC?
A few technical challenges arose during the data analysis. First, we need a robust method to establish the transmission direction between index cases and their close contacts. Due to asymptomatic and pre-symptomatic shedding, index cases were not necessarily the source of infections in these putative transmission events. To infer the direction of transmission, we developed an inference method to estimate the infection time of confirmed cases. Second, disease transmission has a strong spatial-temporal autocorrelation, which imposes difficulty in using statistical models to assess the effects of control measures. We used an established statistical method to account for the spatial-temporal correlation in our analysis.
We found that the turnaround time of contact tracing in NYC was surprisingly short. Statistics indicate that the operation of contact tracing was very efficient. We reconstructed exposure and transmission networks at both individual and ZIP code scales. We found considerable heterogeneity in reported close contacts and secondary infections and evidence of extensive transmission across ZIP code areas. The networks revealed the spatial pattern of SARS-CoV-2 spread and communities that were tightly interconnected by exposure and transmission (Fig. 1). We further found that locations with higher vaccination coverage and lower numbers of visitors to points-of-interest had reduced within- and cross-ZIP code transmission events, highlighting potential measures for curtailing SARS-CoV-2 spread in urban settings.
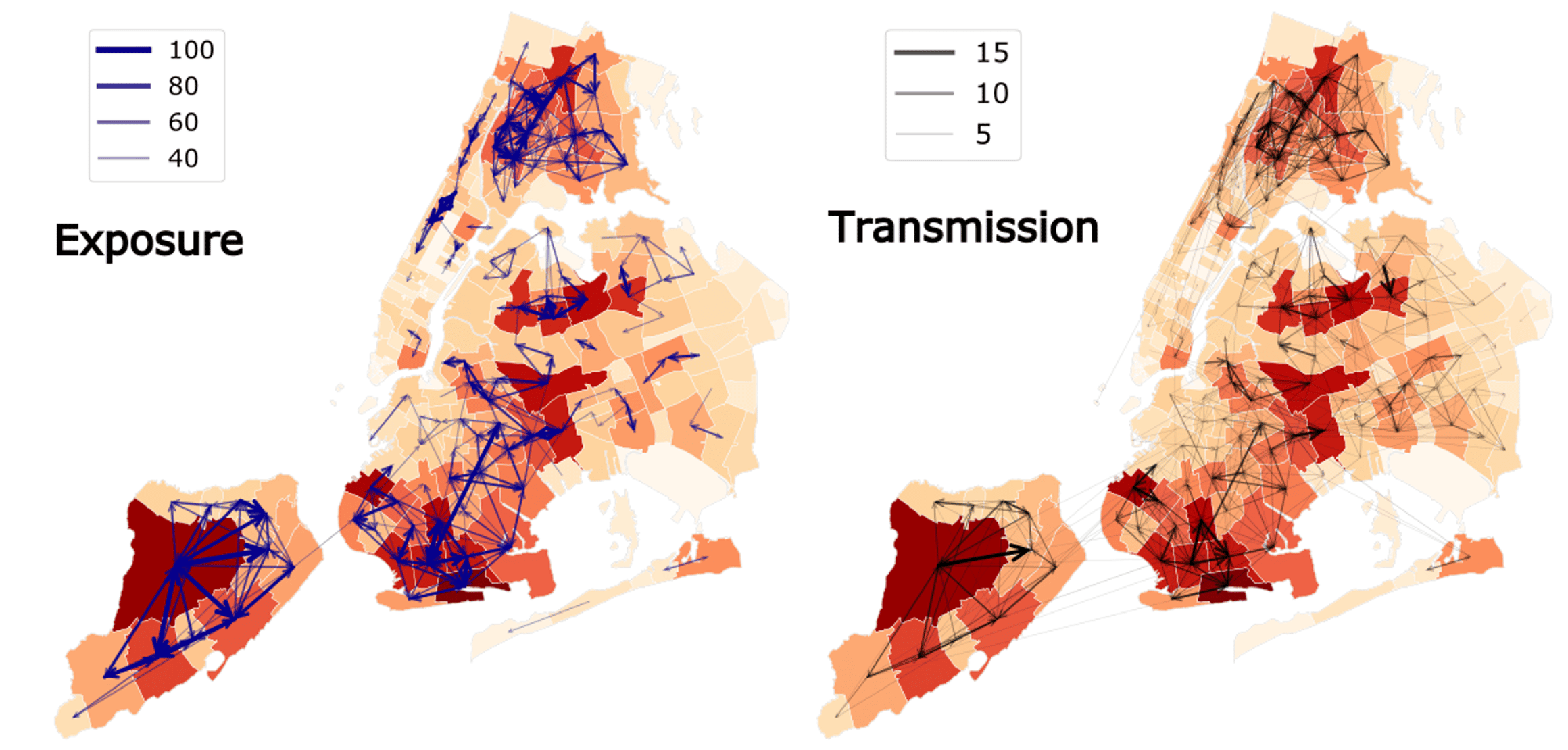
Figure 1. Exposures and transmission events across ZIP codes in NYC identified from contact tracing data. Arrows indicate direction of exposure (from index cases to reported close contacts) and transmission (from index infections to infected contacts). Arrow thickness indicates the number of exposures and transmission events. ZIP code area color represents the cumulative number of confirmed cases during the study period (yellow to red – low to high). To better visualize, exposure links with less than 30 events and transmission links with less than 2 events are not shown on the maps.
This study touches on the critical question of whether operational contact tracing can reduce infectious disease transmission in a real-world setting. Apart from the direct impact of reducing infections through exposure notification and encouraged quarantine, secondary data analysis can also provide insights in intervention designing. For instance, such analysis may inform a better definition of the proper geographical units for observation and interventions based on actual human interactions and disease transmission. Coordinated interventions targeting identified clusters of communities currently supporting the spatial transmission of infectious diseases could potentially produce more effective outbreak control.
Many important questions on contact tracing remain open. For a highly transmissible disease like COVID-19, contact tracing alone may not be enough to eliminate transmission. Exploring a bundle of interventions that can work synergistically with contact tracing to cost-effectively contain an outbreak has a profound implication for pandemic preparedness. How to better design the contact tracing system integrating phone-based surveys and digital techniques (such as app-based services or bluetooth) is important to extend the coverage of contact tracing beyond household members. On the operational side, how to encourage the public to use contact tracing without worrying about privacy issues determines the eventual utility of these tools. Addressing these questions requires expertise from a multitude of disciplines and collaborations between academia, public health authorities and funding agencies.
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in