De novo mutations in mitochondrial DNA of iPSCs produce immunogenic neoepitopes in mice and humans
Published in Bioengineering & Biotechnology

In our lab, we investigate the immune principles of cell transplantation for regenerative medicine. This field is still at the very beginning and many open questions remain. Specifically, “is it necessary and sufficient to generate autologous iPSC-derived cell products to prevent rejection?”. The answer to whether it is sufficient to generate inhertently non-immunogenic cells will then factor in whether it is necessaryto manufacture patient-specific autologous grafts.
Early experience in autologous iPSC-derived retinal pigment epithelial cell transplants showed the difficulties in generating autologous graft cells from a technical stand point. It requires extensive and lengthy manufacturing and in many cases cell products don’t meet basic quality control (QC) standards from a safety standpoint. Although there is still discussion about what’s sufficient for safety QC and standards may be adjusted, predictive assays for efficacy are lacking completely. Specifically for cell rejection, efficacy decreases with the vanishing of graft cells while safety increases.
Experimentally, there have been reports on the fate of autologous or syngeneic cell grafts but mechanistic details remained elusive. We and others have investigated the integrity of the mitochondrial DNA (mtDNA) as possible starting point for autologous graft failure. The mitochondrial DNA is more susceptible for mutations than the chromosomal DNA and heteroplasmy drifts and enrichments may occur and may alter cellular characteristics. While it had been shown previously that some mtDNA mutations lead to energetically disadvantaged progeny, we showed that mtDNA mutations could alternatively or additionally give rise to transplant-relevant neoantigens (Deuse T. Cell Stem Cell. 2015;16:33-8). In our newest paper published in Nature Biotechnology, we now show that such mtDNA mutations can create an immune barrier for autologous iPSC-derived cell grafts.
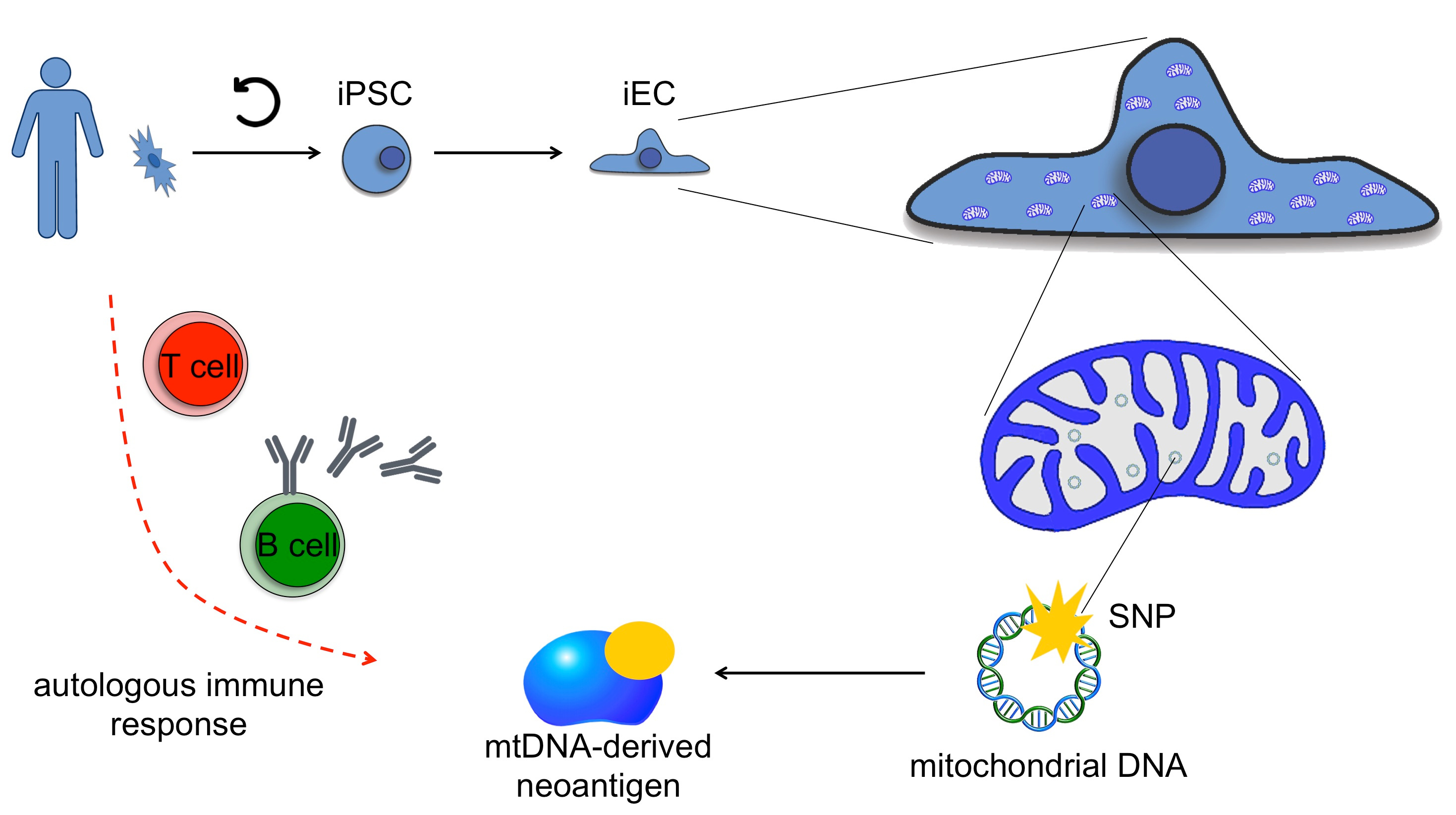
We performed serial mtDNA sequencing of mouse and human iPSCs and showed that the occurrence of neoantigen candidate single nucleotide polymorphisms (SNPs) is common. We arbitrarily defined a threshold for neoantigen candidates based on the mtDNA mutation or heteroplasmy enrichment and validated this as a valuable tool. There appears to be a threshold for the abundance of altered mtDNA-derived proteins necessary to trigger an immune response. Importantly, since in vitroreprograming and culture expansion takes place in the absence of immune surveillance, we believe this is an artificial phenomenon that allows the amplification of cells that would normally undergo immune clearance in vivo.
Whether a neoantigen candidate (solely based on the mtDNA alteration) becomes an immunologically relevant antigen depends on how well the recipient’s major histocompatibility complex (MHC) type can present this epitope. Using very sensitive immune assays, we here show that the immune system in mice and humans detects certain mtDNA-derived neoantigens, whether introduced via allogeneic transplantation or whether they occurred in autologous cells during in vitroreprograming and culture expansion. Most importantly, this detection led to the cytotoxic in vitrokilling of neoantigen-carrying autologous iPSC-derived endothelial cells in mice and humans.
Coming back to our initial question, this study shows that autologous iPSC-derived cell products are not inherently non-immunogenic. But, if autologous cell manufacturing is not sufficient to prevent rejection, is it then necessary to generate autologous cells? No definite answer can so far be given to this question. We believe that the engineering of hypoimmune allogeneic cells might ultimately be the more successful and more economically viable strategy for regenerative medicine. Engineering strategies from our lab (Deuse T. Nat Biotechnol. 2019;37:252-258) and others are encouraging. The combination of iPSC technology with current gene editing capabilities provide us with the tools necessary to design a new class of cell therapy products. We anticipate to see major advances in immune evasion cell technology in the next few years.
Follow the Topic
-
Nature Biotechnology

A monthly journal covering the science and business of biotechnology, with new concepts in technology/methodology of relevance to the biological, biomedical, agricultural and environmental sciences.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in