Detecting RBD with a Home-based Technology
Published in Bioengineering & Biotechnology, Neuroscience, and Protocols & Methods

Good night sleep is crucial for our health, playing a vital role in maintaining our overall well-being. Whether you are a student managing deadlines, a parent juggling between your career and family responsibilities, or just trying to navigate the challenges of daily life, sleep is an important foundation of good mental and physical health. Yet, for many individuals, conditions like sleep apnea, insomnia, REM Sleep Behavior Disorder (RBD), and many others might make sleep anything but restful.
Our paper concerns RBD. RBD is characterized by dream enactments and major body movements during dreaming. Beyond disrupting sleep, RBD is often an early warning sign of serious neurological conditions like Parkinson’s disease, underscoring the need for accessible and accurate diagnostics.
The Challenges of Sleep Diagnostics: To be properly treated, one must be first accurately diagnosed through a sleep study in a sleep laboratory. Imagine undergoing a sleep test in a lab. You arrive at a specialized facility, you are connected to bulky cables and sensors, and then you must spend the night in an unfamiliar environment under observation and video recording. While video-polysomnography setup is the gold standard for diagnosing sleep disorders, it often interferes with the very thing it aims to measure: Your typical sleep. Many people experience the "first-night effect," where the strangeness of the setting disrupts their usual sleep patterns, potentially skewing the results.
The Future is Wearable, Comfortable, and Home-Based: But what if sleep diagnostics did not require a lab at all? Imagine monitoring sleep comfortably at home with the same precision as a lab test. Wearable and wireless technologies are making this a reality, offering solutions that are more comfortable, flexible, and practical. Yet, to have medical validity, sleep monitoring must adhere to very specific standards that are not offered by most wearable systems. Our study utilized a special electrophysiological system developed originally at the Neuro-Engineering lab at Tel Aviv University and now available commercially. It features a thin, dry, flexible adhesive electrode array connected to a compact Data Acquisition Unit (DAU). Followed up by several years of joint research with Prof. Anat Mirelman yielded laboratory and home data which we could then analyse towards better understanding RBD detection at home.
Our Study: Diagnosing RBD starts with understanding REM Sleep Without Atonia (RSWA), a key marker of unusual muscle activity during REM sleep. Normally, muscle tone is suppressed in REM sleep, preventing individuals from physically acting out their dreams. However, in conditions like RBD, muscle tone is not fully suppressed, leading to excessive movements during REM sleep. Measuring RSWA has been a complex and time-consuming task. In our study, we presented a semi-automated algorithm designed to quantify RSWA. By standardizing EMG detection and removing mechanical artifacts, this method analyzes EMG data during REM sleep. Leveraging adaptive thresholds and key features, it streamlines the identification of muscle activity, making the diagnostic process more accurate and automated. We conducted a study involving 55 participants, collecting full-night sleep recordings in both home and lab environments.
Key Findings
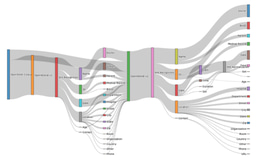
- Consistency across environments (figure a): Sleep micro-structures like RSWA showed a moderate correlation of 0.61 between home and lab environments,
- reinforcing the reliability of home-based testing.
- High sensitivity and accuracy (figure c): The wearable system achieved 83% sensitivity, 79% specificity, and 81% balanced accuracy in detecting RBD patients, suggesting it is a reliable tool for at-home screening.
- Macro-structure variability: Significant differences in macro-structures (e.g., sleep stages, sleep efficiency) between lab and home settings highlight the importance of evaluating patients in their natural sleep environment for a more accurate understanding of their sleep patterns.
What’s Next? We successfully demonstrated the potential of a new wearable sleep technology. Looking ahead, we aim to expand our cohort to include a greater number of participants and consecutive nights. By capturing multiple nights of sleep, we may enable a deeper understanding of night-to-night variability and enhance the ability to screen for RBD. Our aim includes developing a more comprehensive, fully automated algorithm to create an end-to-end solution that will facilitate diagnostic capabilities across diverse populations.
Dreaming Big: This study represents a major step forward in making sleep studies in the realm of RBD more accessible, more reliable, and more patient friendly. As sleep monitoring technology evolves, bringing high precision levels to the home is no longer a dream, it is a reality in the making.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in