Developing the genomic workforce: insights from a national survey
Published in Healthcare & Nursing
Why focus on developing genomics capability in the health care workforce?
Doctors are increasingly using genomic information to screen for, diagnose or manage genetic conditions. Genomics has potential for all areas of medicine and is already being used in areas from reproductive carrier screening to targeted treatments. A capable workforce will be necessary across all specialties for patients to benefit from genomics.
In Australia, more than a million genetics or genomics tests are performed each year (1) but only a small percentage are requested by doctors who specialise in genetics.
We therefore aimed to explore the role of education in supporting doctors to adopt genomic medicine into their clinical practice (2). We surveyed Australian doctors not trained in genetics/genomics, asking about their current and future practice in genomics, confidence, and steps taken to prepare for genomics, such as completing continuing education activities (3).
How can we improve genomics education for health professionals?
Nearly a decade ago, our group of Australian researchers and educators designed a program of collaborative research focused on ways to support development of the workforce for genomic medicine. Numerous studies were conducted to understand the practice and educational needs of a range of health professionals, and to support genetics/genomics educators. We used mixed methods, including consensus methodologies with national and international experts.

As part of our research, we interviewed nearly 90 doctors (4) and over 30 educators (5) to develop a survey for doctors not trained in genetics/genomics (5). The interview data revealed five domains of interest: doctors’ Personal characteristics, their current Practice related to genomics, perceptions of the Proximity of genomics to their practice, their feelings of Preparedness, and their Preferences for service delivery and education. These were our "5Ps" for genomic medicine.
To develop the survey, we identified potential questions from the literature that related to these domains, or created new questions if none existed. We then asked 22 experts in genetics, general medicine, genetics/genomics education, evaluation and implementation science to review questions for relevance, clarity and importance (5). We also cross-referenced each question to the COM-B model for behaviour change, where behaviour is influenced by capability, opportunity and motivation (6).
The survey tool, based in empirical data and informed by relevant theories, has been used by others both locally and internationally (e.g., 7-10), allowing benchmarking of genomics practice, across both time and different regions.
We deployed the survey in Australia in 2019, using multiple strategies to reach doctors in as many specialties, career stages and locations as possible. A snapshot – published previously (3) – highlighted that over half of respondents (54%) were already engaged in some way with genomic medicine, mainly performing tasks associated with pre-test family history taking and counselling. Doctors who responded to the survey expected to perform tasks at all stages of testing in the future, with only a quarter (25%) feeling prepared to practise genomic medicine.
Although 42% of respondents thought that improved genomics knowledge would alter their clinical practice, the same proportion were ‘unsure’. This suggested that a more in-depth analysis of the data could be helpful to inform future education and implementation.
The questions that drove our analyses were:
- What are the differences between doctors who engage with genomic medicine and those who don’t?
- What are the differences between doctors who are confident to practice genomic medicine and those who aren’t?
- Are there any associations between the topics that doctors had learnt about and their confidence, practice and perceptions of genomic medicine?
The findings from these analyses are reported in our recent npj Genomic Medicine publication (11) – the ‘paper behind this blog’.
What did we learn?
We found significant associations between doctors’ engagement with genomics, research experience and genomics education, and their perceptions of genomics and possible delivery models for genomic medicine - referring to a genetics service, requesting genomic testing with support from a genetics service, or requesting testing autonomously.
Doctors engaging with genomics (requesting or referring for genomic testing) were more likely to have completed genomics education in the past year and to have genomics research experience. They were also more likely to prefer to request genomic tests themselves with some additional support from genetics services. For those not previously engaged with genomics, the most common reported reason was being unsure about relevance of genomics to clinical practice.
Doctors’ confidence overall was associated with already being engaged with genomics, having completed education, and having research experience.
Interestingly, there were no associations between career stage and engagement or confidence, suggesting doctors at different stages of their training and career do not need different education programs.
At least half of the doctors who responded to the survey had previously learnt about genomics and its clinical aspects, with fewer learning about genomic technologies or relevant ethical, legal or social implications (ELSI). Importantly, respondents who had learnt about some specific genomics topics were less likely to be confident. This could suggest an interplay between education and confidence, akin to the 'conscious competence' ladder (12), or the Dunning-Kruger effect (13).
How are our findings useful to others?
Understanding the characteristics of doctors who are already engaged with genomics and who feel confident to practice can help educators provide genomics education that is fit for purpose. Our results highlight the need to provide a range of education formats and topics pitched to different levels of competence across a proposed progression.
We developed a model from our data (Figure 2, pictured below) that we hope will help policy makers in genomics as well as educators. The model is informed by our evidence as well as theory. It is pragmatic, acknowledging that health professionals will work across a variety of contexts, with different service delivery models that require different capabilities.
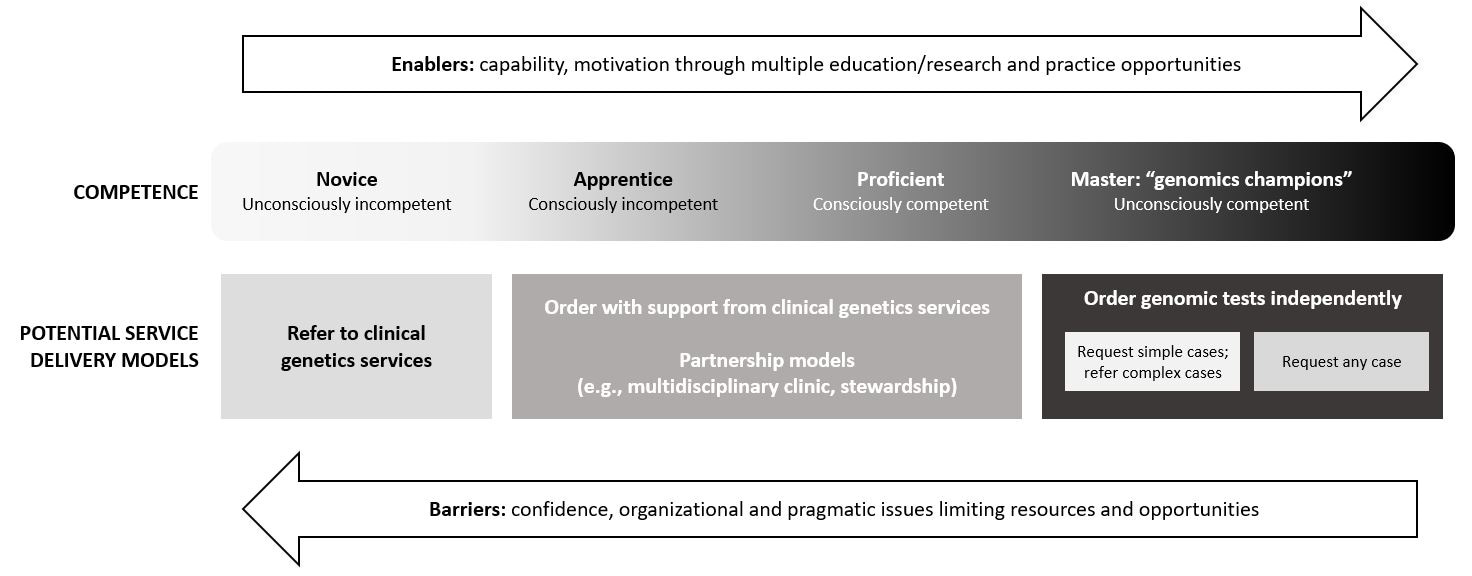
We’re pleased to have received feedback that this model is simple but effective. It took a long time for us to pull out the key messages from the data and the model was revised many times to make it understandable and relatable to a broad readership!
We’re also delighted that people reviewing and already using the model see its usefulness for the wider genomics community, including policy makers, those who influence the implementation of genomic medicine, and other jurisdictions transforming service delivery to accommodate emerging technologies.
The model sits alongside the other tools developed as part of our program to support effective, professional genomics education. These include: a program logic model and template (14), needs assessment surveys (5,15), and reporting standards for genomics education and evaluation (16), plus an evaluation framework that will be published shortly.
References
- Royal College of Pathologists of Australasia. Australian Health Genetics/Genomics Survey 2017 Report of Key Findings to: Department of Health. (Royal College of Pathologists of Australasia, 2019).
- Crellin, E. et al. Preparing medical specialists to practice genomic medicine: education an essential part of a broader strategy. Genet. 10, 789 (2019).
- Nisselle, A., King, E. A., et al. Measuring physician practice, preparedness and preferences for genomic medicine: a national survey. BMJ Open 11, e044408 (2021).
- McClaren, B. J., et al. Preparing medical specialists for genomic medicine: Continuing education should include opportunities for experiential learning. Genet. 11, 151 (2020).
- McClaren, B. J., et al. Development of an evidence-based, theory-informed national survey of physician preparedness for genomic medicine and preferences for genomics continuing education. Genet. 11, 59 (2020).
- Michie, S., van Stralen, M. M. & West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 6, 42 (2011).
- Scheuner, M. T., et al. Genetics professionals are key to the integration of genetic testing within the practice of frontline clinicians. Med. 25(1), 103 (2023).
- Jayasinghe, K., et al. Attitudes and practices of Australian nephrologists toward implementation of clinical genomics. Int. Rep. 6(2),272 (2021).
- Primiero, C. A., et al. Attitudes of Australian dermatologists on the use of genetic testing: A cross-sectional survey with a focus on melanoma. Genet. 13, 3062 (2022).
- Rahma, A. T., et al. Knowledge, attitudes, and perceived barriers toward genetic testing and pharmacogenomics among healthcare workers in the United Arab Emirates: a cross-sectional study. Person. Med. 10(4), 216 (2020).
- Nisselle, A. et al. Investigating genomic medicine practice and perceptions amongst Australian non-genetics physicians to inform education and implementation. npj Genom. Med. 8, 13 (2023).
- Gullander, O. E. Conscious competency: the mark of a competent instructor. Canad Training Methods 7, 20–21 (1974).
- Kruger, J., & Dunning, D. (1999). Unskilled and unaware of it: How difficulties in recognizing one's own incompetence lead to inflated self-assessments. Person. Soc. Psych. 77, 1121 (1999).
- Nisselle, A., et al. Ensuring best practice in genomic education and evaluation: a program logic approach. Genet. 10, 1057 (2019).
- Nisselle, A., et al. Readiness of clinical genetic healthcare professionals to provide genomic medicine: An Australian census. Genet. Couns. 28, 367 (2019).
- Nisselle, A., et al. Ensuring best practice in genomics education and evaluation: reporting item standards for education and its evaluation in genomics (RISE2 Genomics). Med. 23, 1356 (2021).
Follow the Topic
-
npj Genomic Medicine

This is an international, peer-reviewed journal dedicated to publishing the most important scientific advances in all aspects of genomics and its application in the practice of medicine.
Related Collections
With Collections, you can get published faster and increase your visibility.
Artificial Intelligence in Genomic Medicine
Publishing Model: Open Access
Deadline: Jun 23, 2026
Genomics in precision medicine
Publishing Model: Open Access
Deadline: Apr 14, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in