Do Multiple COVID-19 Vaccine Doses Affect Metabolism?
Published in Chemistry, Biomedical Research, and Immunology

Study Overview:
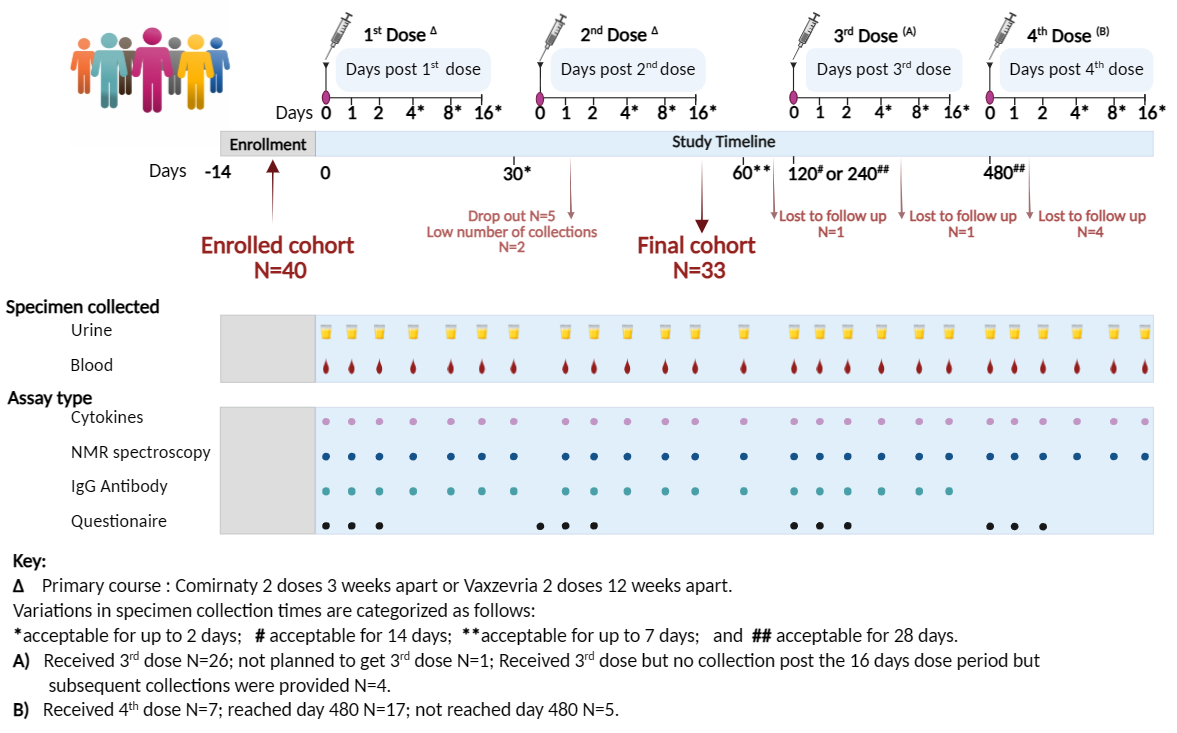
This real-world longitudinal study, conducted in Western Australia, evaluated the metabolic and immunologic responses of 33 individuals who received up to four doses of either Pfizer-BioNTech (Comirnaty™) or Oxford-AstraZeneca (Vaxzevria™) vaccines. We tracked 34 cytokines, 112 lipoprotein markers, and 21 low-molecular-weight metabolites over a period extending up to 480 days after the first dose. Samples were collected immediately before and within two weeks after each vaccination to capture both short- and long-term biological responses.
Key Findings: ![]()
1. Temporary Immune Activation
After vaccination, a short-lived increase was observed in inflammatory cytokines such as IP10 (CXCL10) and MIP-1β. Importantly, these cytokine levels quickly returned to baseline and remained well within normal healthy ranges between doses, indicating a controlled and transient immune response, distinct from the serious inflammatory patterns seen in COVID-19 infections.
2. Metabolic Stability
Metabolic profiling revealed minimal changes following vaccination.
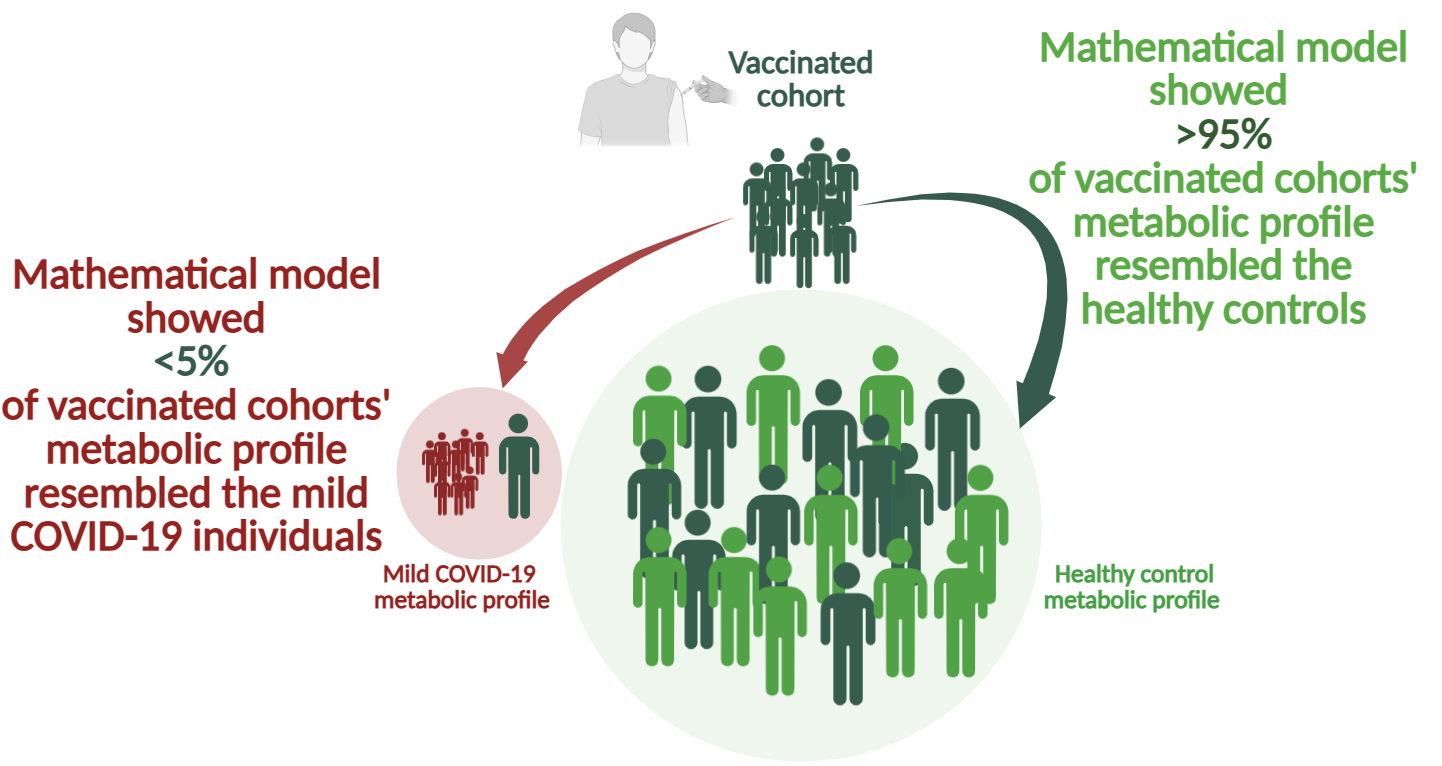
To assess this, the vaccinated cohort's samples were compared to two reference groups:
- Individuals with mild COVID-19 infections (PCR-positive, non-hospitalized), and
- Healthy controls with samples collected before the pandemic.
Using mathematical modelling, we found that over 95% of the vaccinated individuals' blood profiles resembled healthy controls, not those with COVID-19 infection.
Approximately 5% of samples showed metabolic fingerprints more similar to mild COVID-19 cases. Notably, half of these samples came from one individual later diagnosed with long COVID after overseas travel.
Created in https://BioRender.com
3. Small and Isolated Metabolic Shifts
Further analysis found a temporary increase in glutamic acid levels after the third vaccine dose. While intriguing, given glutamic acid’s role in immune regulation and cardiovascular health, the glutamine-to-glutamic acid ratio remained within normal ranges, suggesting no adverse functional impact.
Why It Matters:
This study provides real-world evidence that repeated COVID-19 vaccination does not induce harmful metabolic effects. It offers important reassurance for individuals seeking to stay current with recommended vaccine schedules without fearing long-term metabolic consequences.
Full Study:
The research is published in the Journal of Molecular Medicine:
Longitudinal study on immunologic, lipoproteomic, and inflammatory responses indicates the safety of sequential COVID-19 vaccination
Media:
Dr. Norman Swan discusses the findings on the ABC Health Report.
Listen here
Follow the Topic
-
Journal of Molecular Medicine

This is a renowned journal focusing on basic findings from disease pathogenesis to therapy research across all human diseases.
Related Collections
With Collections, you can get published faster and increase your visibility.
Ferroptosis: From Molecular Mechanisms to Clinical Applications
Ferroptosis is a unique form of regulated cell death driven by iron-dependent lipid peroxidation. Unlike apoptosis, necrosis, or autophagy, ferroptosis involves distinct metabolic and signaling pathways, making it a critical area of study with significant implications for understanding various diseases, including cancer, neurodegeneration, and ischemia-reperfusion injury. Over the past decade, the molecular mechanisms underlying ferroptosis have been extensively studied, revealing potential therapeutic targets that could lead to innovative treatments for a wide range of diseases. Given the substantial growth in research focused on ferroptosis, it is timely to bring together leading experts in the field to present their latest findings and perspectives. This special issue aims to provide a comprehensive overview of the current state of ferroptosis research, spanning from fundamental molecular mechanisms to translational research and potential clinical applications.
The special issue will cover a broad spectrum of topics related to ferroptosis, including but not limited to:
A. Molecular Mechanisms of Ferroptosis: including (1) Role of iron metabolism in ferroptosis. (2) Lipid peroxidation and antioxidant defense mechanisms. (3) Genetic and epigenetic regulation of ferroptosis. (4) Signaling pathways involved in ferroptosis initiation and execution.
B. Ferroptosis in Disease: including (1) Ferroptosis in cancer: potential for therapeutic targeting; (2) Neurodegenerative diseases and ferroptosis.(3) Ferroptosis in cardiovascular diseases, including ischemia-reperfusion injury. (4)The role of ferroptosis in inflammation and immune response.
C. Therapeutic Strategies: (1) Small molecules and natural compounds targeting ferroptosis.(2) Ferroptosis inhibitors and their potential clinical applications. (3) Biomarker development for ferroptosis-related diseases. (4) Preclinical and clinical studies exploring ferroptosis-based therapies.
Keywords: Ferroptosis; Iron metabolism; Lipid peroxidation; Antioxidant defense; Neurodegenerative diseases; Cardiovascular diseases; Therapeutic targeting; Biomarkers; Inflammation; Cell death; Cancer therapy.
Publishing Model: Hybrid
Deadline: Apr 30, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in