Effectiveness of DialBetesPlus, a self-management support system for diabetic kidney disease: Randomized controlled trial
Published in Biomedical Research and General & Internal Medicine
Cover image:
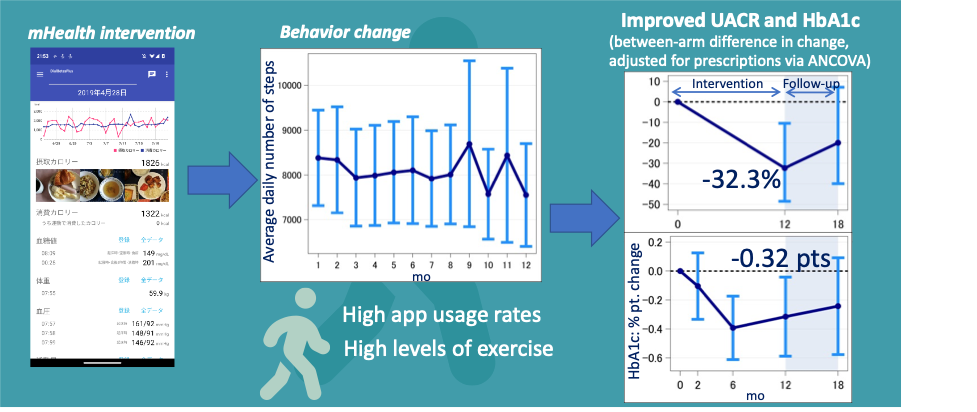
The app provides information on behavior (exercise and diet) as well as intermediate health outcomes (blood glucose, blood pressure, and body weight). Our trial succeeded, as we found that exercise increased, markers of kidney health improved, and glycemic control improved.
What we did and why
Our lab has been developing mHealth interventions that combine wearable devices, smartphone apps, and centralized servers for many years (https://waki-lab.jp). DialBetesPlus aims to help diabetes patients improve their lifestyle so that they can improve their health. In this trial, we used DialBetesPlus in a population with diabetic kidney disease (DKD), as indicated by moderately increased albuminuria, which we defined as a urinary albumin-to-creatinine ration (UACR) of 30-299 mg/g creatinine. DKD is a serious complication of diabetes that is a leading cause of kidney failure. Our trial was among 126 patients over a 12 month intervention (Figure 1.) This is the first trial of an mHealth lifestyle intervention in this population.
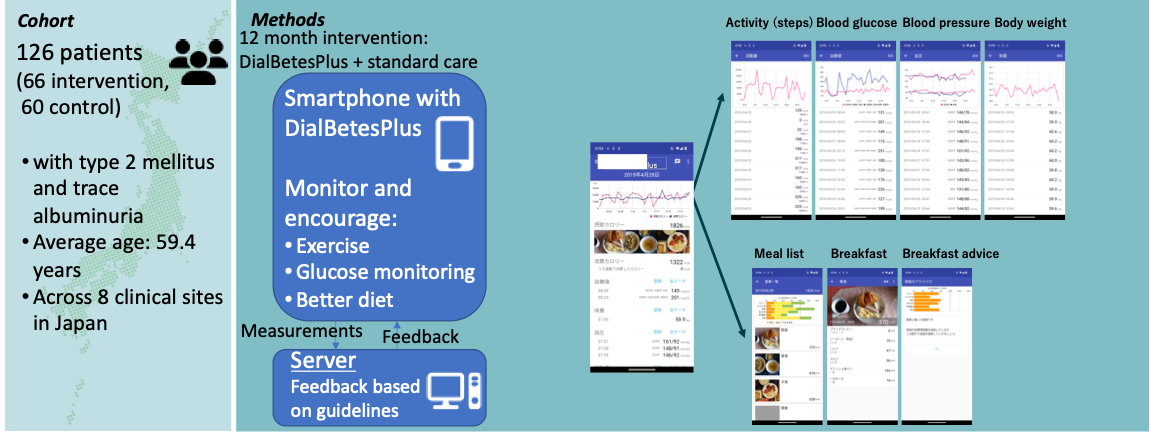
Figure 1. We conducted a large (N = 126 patients with diabetic kidney disease), long (12 month) RCT of DialBetesPlus, an mHealth intervention focused on increasing exercise and improving diet
We designed the study based on what we had learned from our prior efforts as well as the results of others. The mHealth field seems to be going through a phase change. A decade ago, when we were first starting to apply these methods, many were skeptical that “playing around with apps” could be a real medical treatment, and any trial that showed a health outcome was a great success. Today, there have been many such successes, and the bar is higher – we need to show how the intervention led to the health outcome. We expect this trend to extend to requiring the development of deep understanding of what specific elements work and why, so that we can trim out ineffective elements, extend things that work, and try out new concepts to see if they work.
Why does any of this matter? For many diseases, including diabetes, changes in lifestyle such as increasing exercise or modifying diet have been proven to provide significant health benefits as an alternative or addition to pharmacology, but these changes are hard for patients to make. Behavior changes related to healthier lifestyles are more complex than simply taking a medication; devotion of time and energy by patients is necessary for successful and appropriate lifestyle changes. Guidance and feedback from healthcare professionals can help, but this approach is expensive due to time demands on healthcare staff, and these interactions typically happen infrequently, such as at monthly or quarterly visits to a healthcare clinic. Interventions such as DialBetesPlus offer the promise of help that is always there, no matter the time and place, all day and everywhere the patient is, while scaling up economically by avoiding excessive demands on the time of healthcare professionals. The challenge, of course, is developing interventions that are truly effective in real populations.
What we found
We found that our intervention succeeded in improving exercise behavior, with high levels of daily steps (Figure 2.) We found that usage of other features (measuring blood glucose and monitoring diet) was low. Glycemic control, as measured by HbA1c levels, improved 0.3%, as did markers of kidney function, as measured by UACR reductions of 32%. We found a correlation between the number of steps and improvement in HbA1c, and between improvement in HbA1c and improvement in UACR, suggesting that exercise caused the improved health outcomes.
Our study is the first to show an impact on UACR from an mHealth intervention. UACR is a surrogate measure of kidney function, and we found only suggestive improvements in other measures of kidney function. The exact biological mechanism for how improved exercise and glycemic control leads to improved (or perhaps simply maintained) kidney function is not clear, and our results are merely a first step to understanding lifestyle treatment as part of treating diabetic kidney disease.
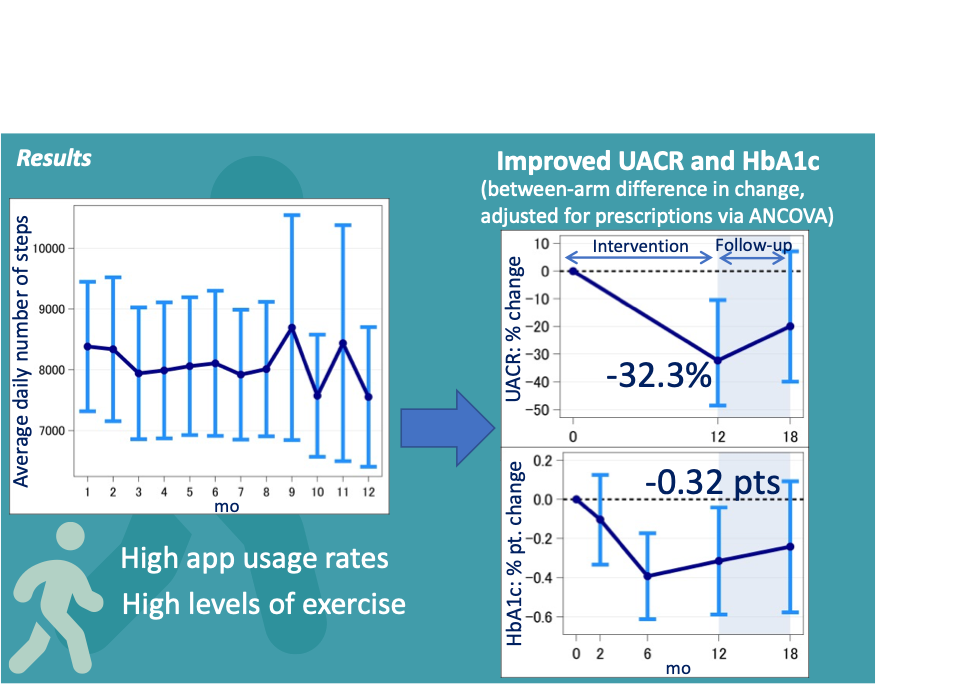
Figure 2. We found significant levels of exercise, improvements in glycemic control (HbA1c), and improvements in markers of kidney function (UACR)
What we learned, and future directions
We learned that our intervention increases exercise in this population. We found that usage of blood glucose measurements was low. We know from anecdotal evidence that patients often dislike using blood stick glucose measurements. It is possible the technologies such as continuous glucose monitoring might lead to better engagement. We found that use of the diet features was very low. Diet is complex, and delivering an intervention that has high engagement and good clinical results is an area needing further work.
Our study was multifactorial, reflecting a physician perspective of using multiple factors that evidence suggests should be helpful. This can make it hard to assess the impact of individual factors, but we did find that exercise is key. We’ve used what we learned with DialBetesPlus in our exercise-focused intervention, StepAdd [Sze W. T. et al. StepAdd: a personalized mHealth intervention based on social cognitive theory to increase physical activity among type 2 diabetes patients. J Biomed Inform. 145:104481 (2023)], which in a pilot led to a larger increase in steps and associated larger improvement in HbA1c. StepAdd is currently being assessed in a formal RCT [Waki K. et al. Efficacy of StepAdd, a Personalized mHealth Intervention Based on Social Cognitive Theory to Increase Physical Activity Among Patients With Type 2 Diabetes Mellitus: Protocol for a Randomized Controlled Trial. JMIR Res Protoc ;13doi:10.2196/53514 (2024)].
There is much work still to be done in this field. As we found, there is a need for diet interventions that lead to high usage levels. There is also a key need to understand why and how interventions lead to the desired behavior change. There is good evidence that grounding an intervention in a theory of behavior change, such as social cognitive theory or the theory of planned behavior, leads to better outcomes than designing interventions without a theoretical basis [Glanz K. & Bishop, D. B. The role of behavioral science theory in development and implementation of public health interventions. Annual review of public health 31:399-418 (2010)], and we are concentrating on using theoretical foundations in our current work.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in