Empowering nurses: exploring self-managed organizations in Indian healthcare
Published in Public Health, Behavioural Sciences & Psychology, and Business & Management
What motivated the study
India’s home-based healthcare sector operates under considerable strain: high patient loads, workforce shortages and deeply hierarchical organisational structures. Nurses often find themselves constrained by bureaucracy, limited autonomy and poor job satisfaction, which in turn affects care delivery and retention. The authors noted a gap in research on how alternative organisational designs—particularly horizontal, self-managed structures—might work in India’s homecare context.
What we did
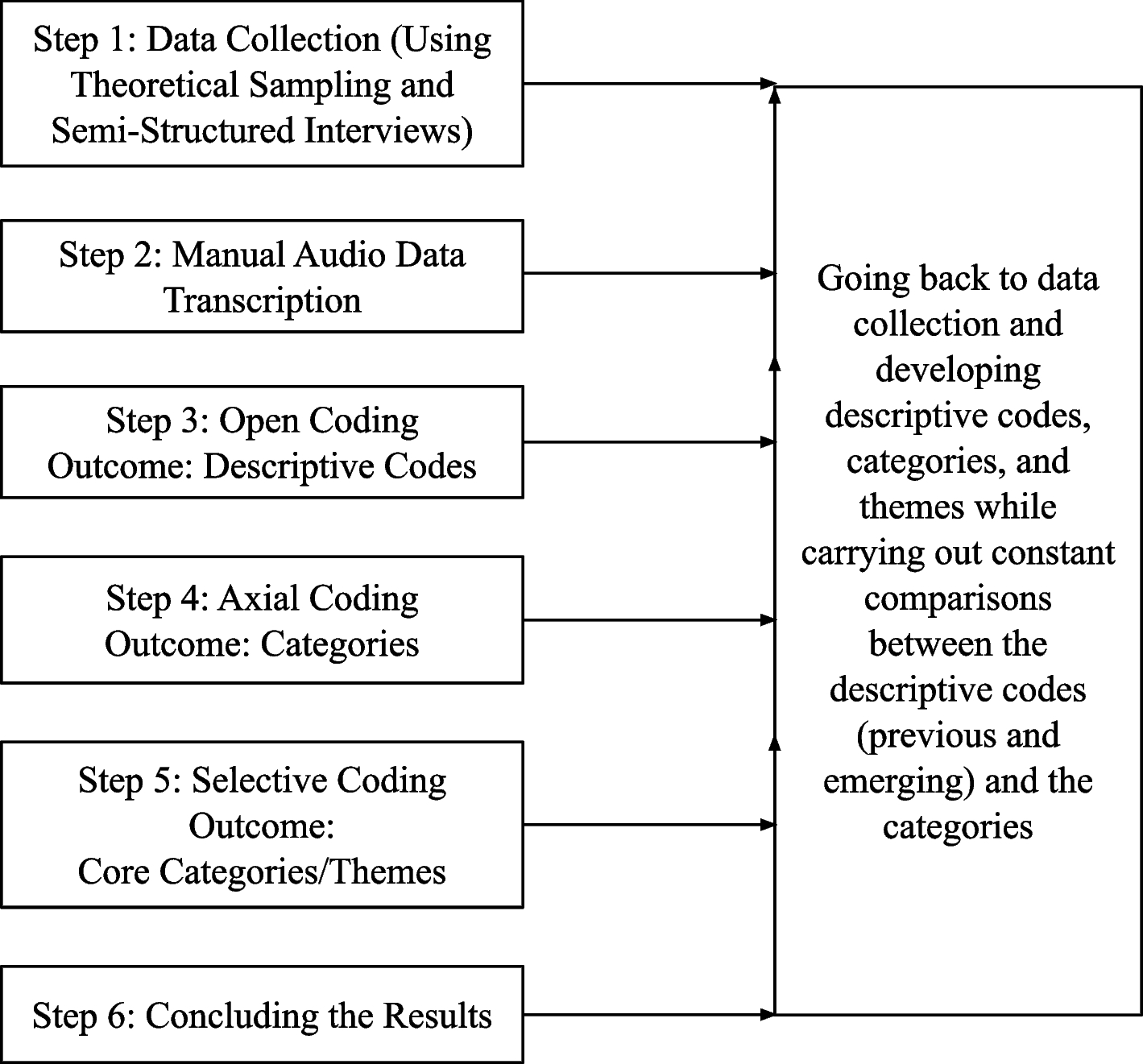
Using a Constructivist Grounded Theory approach, the authors conducted semi-structured interviews with three stakeholder groups: seven nurses, twelve management members and fifteen patients from a self-managed home-care organisation in India. The authors focused on how the structure and culture of the organisation influenced nurses’ experience, how information flows, value systems and conflict resolution worked in a horizontal model, and identified what they term “Qualitative Success Enablers”.
What we found
Three key themes emerged as vital enablers within self-managed organisations in this context:
-
Insightfulness: nurses’ ability to reflect, make sense of complex patient situations, adapt their practices and find meaning in what they do.
-
Enhancing Nursing Experience via Job Enrichment: provision of autonomy, skill variety, feedback and role-rich tasks lifted the experience of nursing from routine execution to engaging professional work.
-
Autonomy-Enabled Intrapreneurship: when nurses were empowered to act as intrapreneurs—identifying improvements, taking initiative, shaping their job design—the entire organisation benefitted in responsiveness and satisfaction.
The case organisation managed to fare well even during the pandemic’s acute phases, suggesting that the self-managed model helped cope with uncertainty better than hierarchical incumbent models.
Why this matters
For management scholars and practitioners, this study offers a compelling example of how organisational design matters in high-stakes, service-intensive contexts like homecare. It challenges the assumption that hierarchical oversight is the only way to ensure quality and efficiency. For Indian healthcare systems and similar emerging-economy settings, it implies that decentralising authority, trusting nurses, enriching job roles and enabling innovation may yield gains in service quality, employee satisfaction and resilience.
What to watch out for
The model doesn’t come without challenges: self-managed structures need strong trust, clarity about roles, supportive coordination mechanisms, and perhaps digital tools to compensate for the reduced traditional oversight. Cultural and institutional legacies in India may slow or complicate transition. The authors note that more work is needed to test how scalable this model is, how long-term outcomes play out, and how it works across diverse geographies and patient populations.
This research takes a bold step by exploring an organisational alternative—self-managed teams—in the typically rigid world of Indian homecare nursing. What emerges is a story not just of flattening structures, but of empowerment, reflection, and intrapreneurial nursing, where the practitioner becomes a designer of their work and the organisation becomes a platform for innovation rather than control.
Follow the Topic
-
BMC Nursing

This is an open access, peer-reviewed journal that considers articles on all aspects of evidence-based nursing care; nursing research methods; nursing service delivery, utilization, and evaluation; nursing administration and human resources.
Related Collections
With Collections, you can get published faster and increase your visibility.
Evidence-based practice in nursing
BMC Nursing is calling for submissions to our Collection, Evidence-based practice (EBP) in nursing. As the field continues to evolve, EBP in nursing remains essential for ensuring high-quality care and advancing best practices. EBP integrates the best available research, clinical expertise, patient values, and non-empirical evidence to guide nursing practices, ultimately enhancing outcomes. As healthcare grows more complex, the need for robust EBP models becomes increasingly critical. These frameworks empower nurses to navigate clinical challenges effectively, ensuring that their practices are grounded in the most current and relevant scientific knowledge.
Emphasizing evidence-based practice within nursing is essential for improving healthcare delivery and patient safety. Applying systematic reviews in practice, promoting the use of clinical practice guidelines, and integrating technology for improved data collection and analysis support nurses in providing high-quality care. These practices not only empower nurses but also encourage collaboration among healthcare professionals, leading to a more unified approach to patient care. Continued focus on EBP will not only enhance professional development but also contribute to the ongoing improvement of healthcare systems.
Future advancements in EBP in nursing may include the development of artificial intelligence tools to support clinical decision-making, the creation of personalized care plans informed by genetic data, and enhanced training programs that equip nurses to navigate evolving healthcare landscapes. As research in both EBP and AI continues to progress, we anticipate a shift toward more data-driven, patient-centered nursing practices that will transform the quality of care.
We call for studies and integrative reviews contributing to the examination of topics relating to evidence-based practice in nursing, including but not limited to:
Implementation of clinical practice guidelines or evidence-based interventions in nursing care and associated metrics
Role of technology in evidence-based practice in nursing
Training and education in evidence-based practice
Challenges or barriers nurses face in adopting evidence-based practices
Research focused on practical solutions and policy development related to evidence-based nursing
Methodology innovation for evidence-based practice in nursing
Stakeholder engagement in evidence-based practice in nursing
Leadership in evidence-based practice in nursing
Evidence-based practice in nursing from a global perspective in resource-limited settings
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Mar 16, 2026
Addictions nursing
BMC Nursing is calling for submissions to our Collection, Addictions nursing. The prevalence of risky substance use, addiction, and substance use disorders (SUDs) has emerged as a significant public health crisis affecting millions globally. Nurses, as frontline healthcare providers, are uniquely positioned to play a pivotal role in both the prevention and treatment of these disorders. Their involvement extends from screening and early intervention to providing compassionate care and education for patients and their families. As the landscape of addiction continues to evolve, understanding the multifaceted role of nurses in addressing SUDs and behavioral addictions is essential for improving patient outcomes and enhancing recovery support.
The urgency of addressing addiction and SUDs cannot be overstated, particularly in light of recent trends that show an increase in opioid and alcohol use, and other substance- and behavior-related issues. Nurses have made significant contributions to the development and implementation of evidence-based practices for managing addiction, including motivational interviewing, harm reduction strategies, and integrated care models. Furthermore, advances in telehealth have enabled nurses to reach underserved populations, providing critical support and resources for those experiencing addiction. Ongoing scholarship is vital to enhance nursing education, practice and research to refine intervention strategies, and promote collaborative care approaches that encompass the complexities of addiction.
Future advancements in nursing related to addiction and SUDs may include the integration of technology, such as artificial intelligence and telehealth platforms, to deliver personalized care. Additionally, increased collaboration between healthcare professionals, policymakers, and community organizations could foster comprehensive support systems. As research in this area progresses, we can anticipate the development of innovative training programs for nurses that focus on trauma-informed care and culturally humble practices, ultimately leading to better health outcomes for individuals impacted by addiction.
We call for manuscripts contributing to the examination of topics relating to addictions nursing, including but not limited to:
- Innovative nursing interventions for substance use disorders and other behavioral addictions (e.g., food, internet, sex, gambling)
- The role of technology in addiction treatment
- Nurse-led harm reduction strategies
- Education and training for nurses in addiction care
- Implementation and evaluation of evidence-based practices
- Nurse-led addiction policy analysis
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 05, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in