Examining hospitalisation and mortality risk of SARS-COV-2 variant omicron sub-lineage BA.2
Published in Healthcare & Nursing
In January 2022, a sub-lineage of the Omicron variant (BA.2) was identified in England. It was found to be more transmissible than the BA.1 sub-lineage [2], which was the previously dominant variant in England at the end of 2021. As variants of COVID-19 evolve, their genetic mutations may result in different characteristics when spreading through a population such as a change in transmissibility or severity. Understanding the severity of different strains of COVID-19 can inform decision making in public health policy and help healthcare systems in planning.
The Omicron BA.1 sub-lineage had previously been found to have reduced risk of severe outcomes of death and hospitalisation compared to the prior dominant variant in England, Delta [3].
As the BA.2 sub-lineage was rapidly becoming the dominant circulating virus variant in England, and available evidence on the severity of BA.2 was limited to small studies which provided inconsistent results, there was a need for a large national study to be undertaken to provide more precise evidence. The primary aim of our study was to determine the relative risks of hospitalisation and death for Omicron BA.2 compared to BA.1.
The UK Health Security Agency (UKHSA) holds information on COVID-19 positive tests in England, as well as COVID-19 mortality surveillance - identifying those who die following a COVID-19 positive test. The majority of hospital health services in England are provided by the National Health Service (NHS), and information on these admissions was also available to UKHSA.
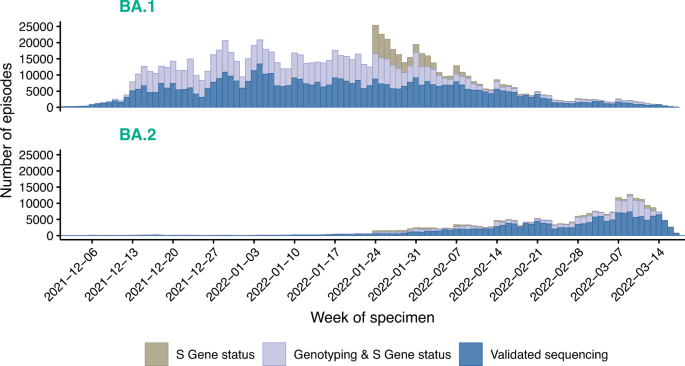
In order to identify cases with the BA.2 sub-lineage and those with the BA.1 sub-lineage, we used available information on genetic sequencing, genotyping and/or S-Gene status. Whilst sequencing was able to identify Omicron sub-lineages, genotyping could only tell us that the case was an Omicron variant and not distinguish the sub-lineage. However, the BA.2 sub-lineage exhibits S-gene target positivity (SGTP) and the BA.1 sub-lineage has S-gene target failure (SGTF). On cases who had a S-Gene result, this could be used in tandem with genotyping to identify the sub-lineage. From 24th January onwards, the positive predictive values of SGTF/SGTP to call BA.1/BA.2 were ≥95% and S-Gene status alone could be used to categorise cases. 258,875 BA.2 and 984,337 BA.1 cases were included in the study.
Cox regression models were used to estimate hazard ratios for the three outcomes: any hospital attendance within 14 days of the positive test, a hospital admission of two or more days within 14 days of the positive test, and death from any cause within 28 days of the positive test. The models were stratified for confounders considered to be important a priori: exact specimen date, area of residence, age group and vaccination status. Stratification methods are analogous to matching, but has the benefit of using all potential matches, unlike e.g. matched cohort analyses that consider a fixed number of matched cases with the comparison variant to each case with the new variant. However, just as with matching, there is a cost of loss of precision when stratifying for a large number of covariates compared to methods based on regression modelling that use no matching or stratification. We additionally used regression methods to adjust for within-age-group residual differences in exact age, sex, ethnicity, index of multiple deprivation (IMD) quintile and within-IMD-quintile residual differences in exact IMD rank, and reinfection status.
We found that the risk of severe outcomes following infection with BA.2 was slightly lower or equivalent to the BA.1 sub-lineage of SARS-CoV-2 Omicron. The BA.2 cases were found to have approximately a 20% reduction in risk of death compared to BA.1, a 12% reduction in risk of hospital admission of 2 days or longer, and roughly similar risks of any hospital attendance.
We were interested in examining the severity of BA.2 infections compared to BA.1 infections within the same age groups, to understand if BA.2 outbreaks could affect some age groups differently than BA.1 outbreaks. Previous studies have shown that the reduced severity of Omicron compared to Delta was mostly found in older age groups, and young children experienced similar, low levels of risk of severe outcomes from either variant [2]. In our study, we found that the reduction in risk for hospital admission was seen in adults between 40-79 years whilst children and those over 80 years of age experiencing similar risk of severe outcomes with either sub-lineage.
We were also interested in if any differences in relative severity were consistent regardless of acquired immunity through vaccination or having had a known prior COVID-19 infection. This would help us understand if sub-lineage-specific differences in evasion of previous immunity would contribute to differences in risk of severe outcomes between sub-lineages. Reassuringly, the results indicated no clear differences by vaccination or past infection status, although we acknowledge that there was low precision to detect such differences due to limited number of events in some subgroups.
Overall, it was reassuring to see the analysis suggests no greater risks of severe outcomes from Omicron sub-lineage BA.2 compared to BA.1. Our large national study has supported the examination of severity in different age groups which had not previously been well described. These results add to the global body of evidence on SARS-CoV-2 variants’ impact on disease severity, and highlights the importance of timely assessment of the severity of new virus variants as they evolve.
References
[1] Webster, HH. et al. Hospitalisation and mortality risk of SARS-COV-2 variant omicron sub-lineage BA.2 compared to BA.1 in England. Nat. Commun. (2022).
[2] Fonager, J. et al. Molecular epidemiology of the SARS-CoV-2 variant Omicron BA.2 sub-lineage in Denmark, 29 November 2021 to 2 January 2022. Eur. Surveill. 27, pii=2200181 (2022).
[3] Nyberg, T. et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B. 1.1. 529) and delta (B. 1.617. 2) variants in England: a cohort study. Lancet 399, 1303–1312 (2022).
Follow the Topic
-
Nature Communications

An open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences.
Related Collections
With Collections, you can get published faster and increase your visibility.
Women's Health
Publishing Model: Hybrid
Deadline: Ongoing
Advances in neurodegenerative diseases
Publishing Model: Hybrid
Deadline: Mar 24, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in