First “Steps” in a Digital Clinical Trial of Wearables
Published in Healthcare & Nursing, Bioengineering & Biotechnology, and Biomedical Research
The recent global health situation rapidly accelerated the adoption of digital clinical trials. Traditional in-person approaches shifted to remote practices, leading to new opportunities as well as challenges. From navigating virtual consent to developing digital endpoints, this blog shares lessons we learned through a recently concluded remote, digital clinical trial – the VALENTINE study.
Consent and Enrollment: Deploying the remote consent and enrollment process begins with a virtual or phone-based explanation of the trial to potential participants. Ensuring individuals fully understand the trial is essential for both ethical reasons and to guarantee reliable results. This necessitates a simple, digital platform where participants can sign their consent, followed by a seamless onboarding process. The first lesson we learned was that digital literacy doesn't strictly correlate with age. Participants showed a high level of competence across age ranges and were generally able to enroll via phone. Despite this, it was useful for us to conduct video or screenshare calls at times to demonstrate multi-step procedures, supplementing verbal instructions as needed. This can be time-consuming, and investigators need to be prepared for it.
Engagement: Maintaining participants’ engagement in any clinical trial can be challenging. However, this can be even more difficult when you don’t have a personal connection with participants as often emerges from face-to-face encounters. We tried to solve this via contextually tailored messages, personalized with participant’s names, and proactive involvement of the clinical team in cardiac rehabilitation (who the participants trusted). Little things made a difference in our experience. For example, we avoided having study text messages “blocked” or ignored by participants by having the study phone number saved as a known contact (i.e., "VALENTINE Cardiac Team").
A clear insight was the necessity of monitoring participant adherence. We did this in two ways. First, we delivered automated text messages to participants who were not wearing their smartwatches as frequently as requested. In addition to this passive strategy, we employed active monitoring of participant adherence though a dashboard. Here, we tracked metrics such as watch wear time and study task completion, allowing study coordinators to re-engage participants through phone calls as needed. Despite the appeal of a completely passive strategy, continuous engagement by our study team members remained essential. A technical support line also became crucial, even if it was occasionally needed for general device-related issues. At times, we served much like a “help” desk for a tech company, though we attempted to minimize assistance with non-study related tasks to the extent this was possible. We also learned that participants in control groups also need tasks assigned to ensure sufficient use of the mobile application, which was necessary to ensure their data were syncing routinely considering study endpoints were also digital.
End of Study Procedures: At the study's end, there's distinct importance in supporting participants with both disengagement from the trial and removing relevant mobile applications from their devices. This ensures there's no inadvertent third-party data capture once the trial culminates. Privacy is a major concern, and we felt it was our responsibility to ensure that participants understood that when the study ended, we were no longer collecting their information without their permission, but other third parties could continue to collect information if those mobile applications were not deleted (i.e., smartwatch associated applications).
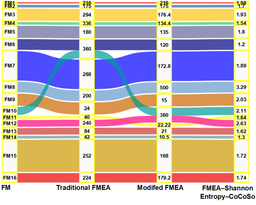
Study endpoints/analysis: In our trial, endpoints included a six-minute walk test, step count, and routine surveys. The six-minute walk test required meticulous coaching and concise instructions to ensure uniformity in approach. Step count, while simple to capture, depends significantly on participant compliance and wear time of the tracking device. A critical learning point was the realization that the field lacks standardization regarding seemingly simple calculated metrics such as wear time. We found various standards used in the published literature for commercial devices. We conducted several sensitivity analyses that evaluated wear time using steps, proprietary device-specific assessments of wear time, and heart rates counts, amongst others. Standard norms and practices still need to be developed in this aspect. Finally, surveys provided a formidable method of data capture, with high levels of compliance and accuracy.
In conclusion, the digital shift of clinical trials has indeed brought about its set of challenges. However, by learning from the hurdles and using the insights brought forth in this trial, future clinical studies can be more efficient, effective, and accessible.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in