Hidden Threat: Mycoplasma genitalium Infection in Pregnancy Linked to Lower Birth Weight Babies
Published in Microbiology, General & Internal Medicine, and Public Health

Explore the Research
Just a moment...
www.cell.com needs to review the security of your connection before proceeding.
Sexually transmitted infections (STIs) and bacterial vaginosis (BV) are common infections that cause a substantial health burden. In pregnancy, some infections can increase the risk of miscarriage, preterm birth, lower-birthweight babies, stillbirth, and serious newborn morbidity (such as blindness or congenital abnormalities) or mortality. M. genitalium is increasingly recognized as a pathogenic STI with the potential to cause cervicitis, endometritis, pelvic inflammatory disease, and infertility in women, as well as urethritis in men. However, the impact of M. genitalium infection on pregnancy outcomes remains poorly understood.
Our study and what we found
Associations between birthweight and M. genitalium and other STIs (Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis) and BV in pregnancy were examined in over 400 maternal-newborn pairs from a prospective longitudinal cohort study in Papua New Guinea in the South-West Pacific region.
When compared to uninfected women, we found that , M. genitalium and N. gonorrhoeae infections were associated with lower birthweight in an adjusted analysis controlling for confounders and covariates. The association for C. trachomatis was less clear, and T. vaginalis and BV were not associated with lower birthweight.
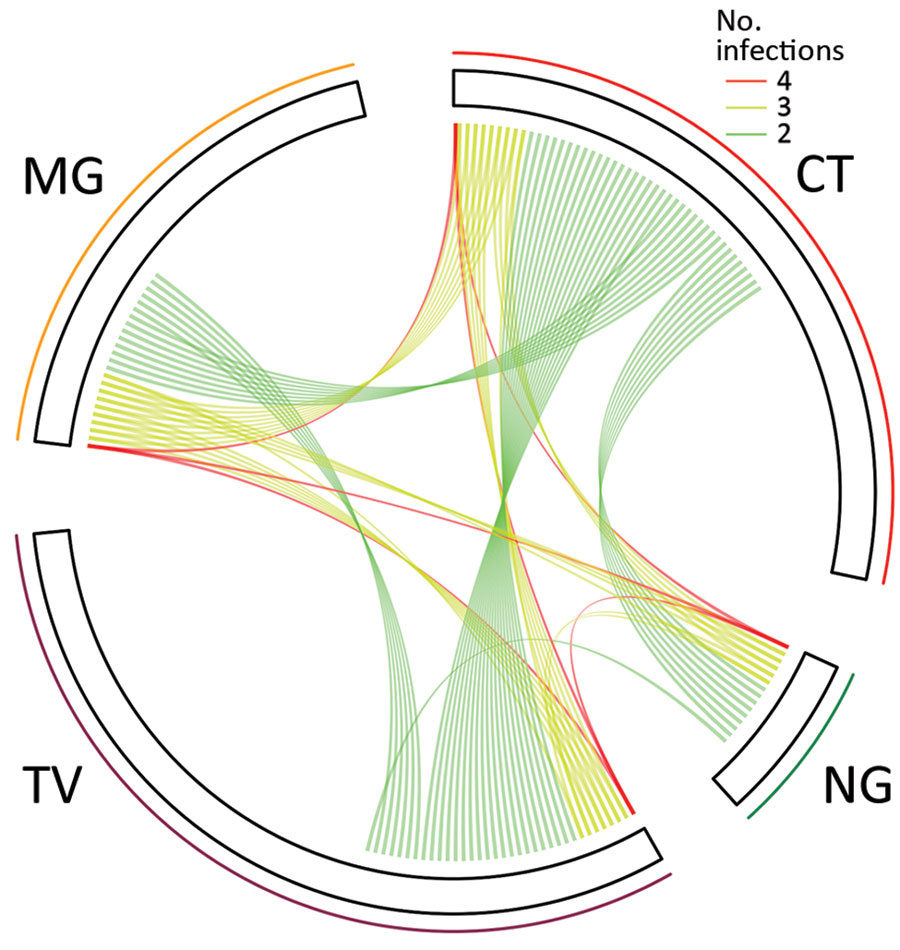
Prevalence of infections was high for M. genitalium (13.9%), N. gonorrhoeae (5.0%), and C. trachomatis (20.0%) and co-infections were frequent. Larger negative impacts on birthweight occurred with co-infections of M. genitalium, N. gonorrhoeae, and/or C. trachomatis.
These findings are important because lower birthweight indicates an increased risk for serious adverse outcomes, and the risk of stillbirth, newborn and infant mortality, and morbidity progressively increases as birthweight decreases. Therefore, addressing treatable factors that can result in lower birthweight is important for reducing the risk of infant morbidity and mortality and improving pregnancy outcomes.
Globally, most recommendations for routine screening in pregnancy do not currently include testing for M. genitalium unless the person is symptomatic. In our study setting, treatment of STIs predominantly relies on syndromic management without access to diagnostic tests due to limited resources; however, more than 80% of women with an STI in pregnancy are asymptomatic and are therefore unlikely to be correctly treated with this approach.
Conclusion
Lower birthweight is a major risk factor for infant mortality and morbidity. Our data provide important new evidence that M. genitalium infection in pregnancy may be causing harm and contributing to lower birthweight and that co-infections appear to lead to an even greater reduction in birthweight. Clinical trials of early diagnosis and treatment of M. genitalium in pregnancy, or treatment of M. genitalium and other STIs prior to conception, are priorities to identify effective strategies to reduce the impact of these infections on reproductive health and adverse pregnancy outcomes and inform public health policy on M. genitalium.
Schematic figure showing an overview of the study and findings
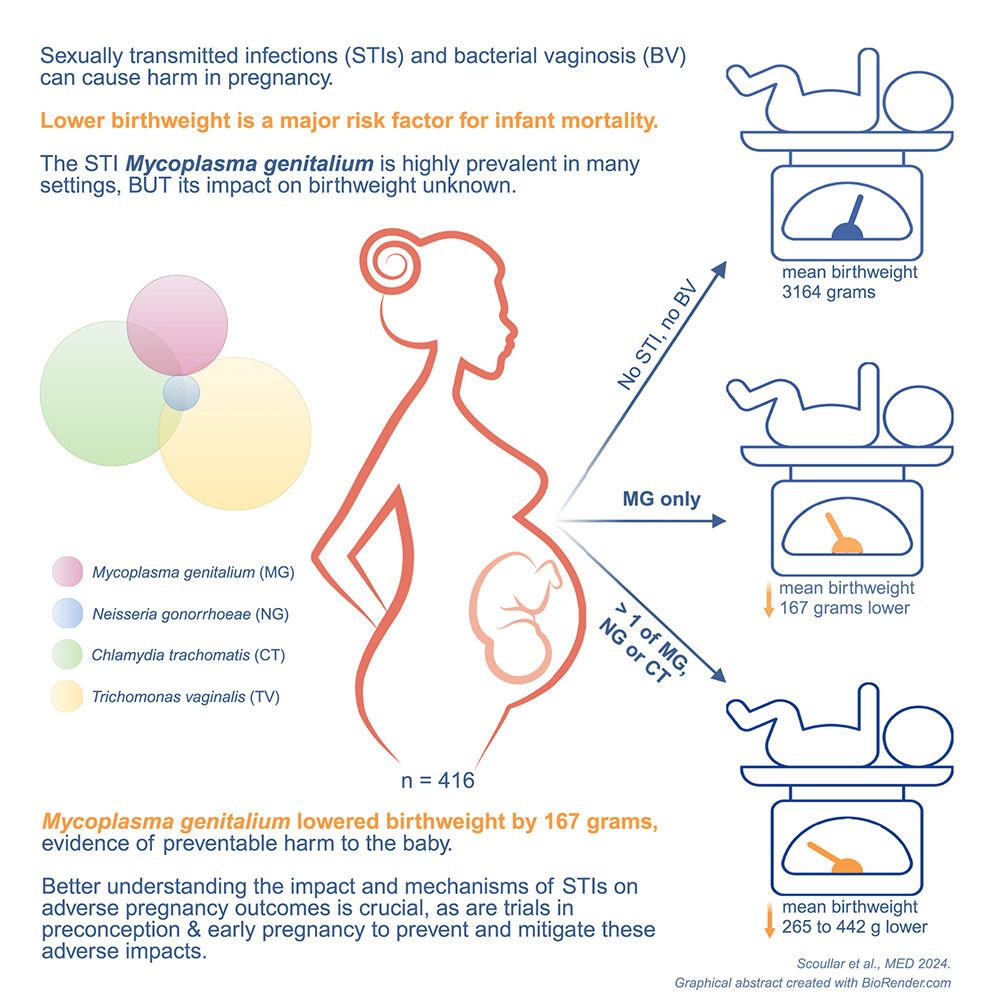
Figure: Relationships among sexually transmitted infections in pregnant women. Each line indicates >2 concurrent infections in 1 participant. The length of each sector corresponds to the number of monoinfections. MG, Mycoplasma genitalium; CT, Chlamydia trachomatis; NG, Neisseria gonorrhoeae; TV, Trichomonas vaginalis. From https://wwwnc.cdc.gov/eid/article/27/3/20-1783_article
Full article can be found here:
Mycoplasma genitalium in pregnancy, including specific co-infections, is associated with lower birthweight: A prospective cohort study
https://www.cell.com/med/fulltext/S2666-6340(24)00211-3?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS2666634024002113%3Fshowall%3Dtrue
Related paper




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in