HIV & SARS-CoV-2 Hybrid Immunity
Published in Microbiology and Immunology

Early in the pandemic, researchers were uncertain how PLWH would respond to COVID-19. Over time, studies showed that individuals with low CD4 T-cell counts were more susceptible to severe outcomes from the infection.
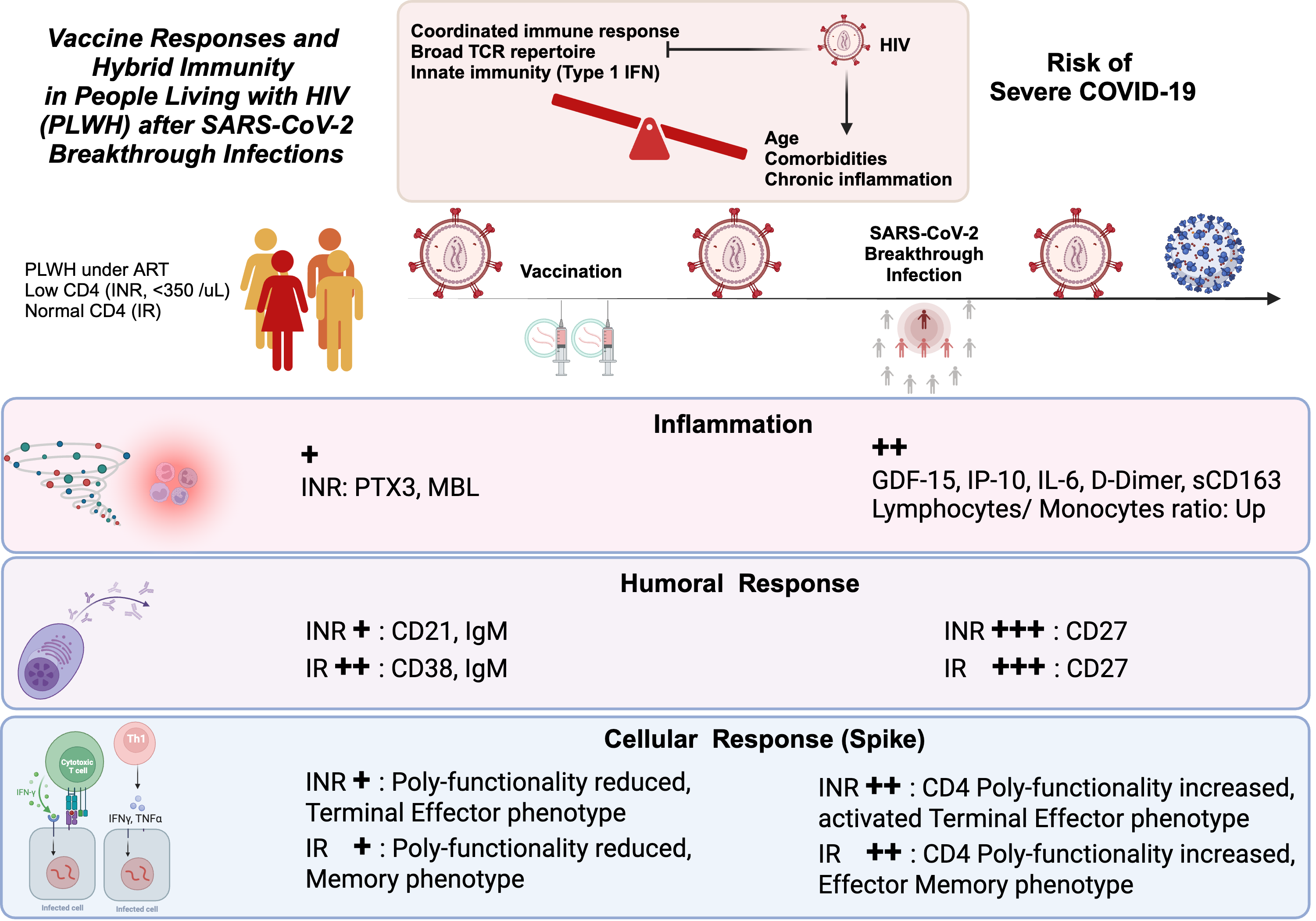
Among PLWH, a specific group known as immune non-responders (INR)—those who, despite successful HIV treatment, are unable to rebuild their CD4 T cells—are at even higher risk. These individuals face not only HIV-related conditions but also a higher likelihood of complications from COVID-19. Research reveals that INR with CD4 counts below 200 cells/mm³ are more prone to severe COVID-19 outcomes compared to immune responders (IR) who have higher CD4 counts. Moreover, INR typically have impaired vaccine responses, including to the COVID-19 vaccines.
How HIV Impacts Immunity
HIV attacks CD4 T cells, weakening the immune system's ability to fend off infections. Even in PLWH on effective antiretroviral therapy (ART), chronic inflammation and immune activation can persist, complicating how they respond to both natural infections and vaccines. This is especially true for INR, whose immune responses are often unpredictable.
Investigating Vaccine Responses in PLWH
Our study set out to explore how PLWH, particularly INR, responds to the COVID-19 vaccines and breakthrough infections (BTI) with variants of concern (VOC). By comparing the immune responses of INR, IR, and healthy donors (HD), the researchers uncovered important findings about how these groups react to the virus and the vaccines.
One key discovery was that INR tends to develop weaker antibody responses post-vaccination. About half of INR participants failed to generate sufficient IgG antibodies, which are essential for neutralizing COVID-19. However, despite these lower antibody levels, INR still maintained their cellular immune responses, which play a critical role in fighting off infections. After experiencing a BTI, antibody levels rose in both INR and IR, though INR’s response remained less robust.
The Role of B Cells and CD4 Counts in Vaccine Response
HIV can impair B-cell function, making it more difficult for INR to produce the antibodies needed to fend off infections. Research shows a clear link between CD4 counts and vaccine effectiveness in PLWH. Lower CD4 counts result in significantly weaker responses, especially in older individuals. Despite this, additional vaccine doses have been shown to improve antibody responses in many immunocompromised individuals, including INR.
The study found that while INR may struggle to mount a strong antibody response after the first two doses of the vaccine, booster doses could potentially enhance their immune protection. Still, questions remain about how long INR can maintain neutralizing antibodies after a BTI and their vulnerability to future variants.
T-Cell Immunity: A Critical Defense
The study also examined T-cell responses, a crucial part of the immune defense. Even though INR showed weaker antibody responses, their T-cell responses to COVID-19 remained relatively strong. However, some INR still failed to develop an immune response to parts of the virus beyond the Spike protein, with around 30% of vaccinated INR showing no significant T-cell response at all.
T-cell responses tend to be more resistant to viral mutations than antibodies, meaning that even when antibody levels are low, T-cells could still help prevent severe disease. Previous studies suggest that SARS-CoV-2-specific T-cell memory can last for around six months, providing some level of protection even after antibody levels wane.
While T-cell immunity in INR remained relatively strong, qualitative defects were noted in their SARS-CoV-2-specific T cells, especially after BTI. These defects included reduced polyfunctionality (the ability of T cells to perform multiple functions), higher expression of senescence (CD57, GPR56), and exhaustion markers, like PD-1, which could impact the durability of the immune response and increase the risk of long-term health complications, such as long COVID.
Chronic Inflammation and COVID-19 in PLWH
HIV is known to cause chronic inflammation, even in those on ART. This inflammation persisted in vaccinated PLWH after BTI, although INR experienced milder symptoms than those with severe COVID-19.
Challenges and Future Directions
While the study offers valuable insights, there were some limitations. The sample size, particularly for INR, was small, and most participants had well-controlled HIV. Additionally, most individuals had already received two doses of the COVID-19 vaccine, making it difficult to assess how vaccines perform after primary infection or against severe disease in PLWH with very low CD4 counts.
In conclusion, this study underscores the importance of T-cell immunity in PLWH, particularly INR, even in the face of reduced antibody responses. It highlights the need for ongoing booster vaccinations and monitoring to ensure protection against future variants. Given the complex relationship between HIV, immune activation, and chronic inflammation, staying on top of ART adherence and timely vaccinations is critical in limiting the impact of COVID-19 in PLWH, especially those with weakened immune systems.
By shedding light on the immune response in PLWH, this study emphasizes the need for continued research and tailored healthcare strategies to protect vulnerable populations from the long-term effects of COVID-19.
Follow the Topic
-
npj Vaccines

A multidisciplinary journal that is dedicated to publishing the finest and high-quality research and development on human and veterinary vaccines.
Ask the Editor - Immunology, Pathogenesis, Inflammation and Innate Immunity
Got a question for the editor about the complement system in health and disease? Ask it here!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Lipid nanoparticle (LNP)-adjuvanted vaccines
Publishing Model: Open Access
Deadline: Feb 19, 2026
Therapeutic HPV vaccines
Publishing Model: Open Access
Deadline: Jun 30, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in