How can we prevent the emergence of a vaccine resistant variant?
Published in Social Sciences
The COVID-19 pandemic has been profoundly affected by human interventions aimed at limiting its damage. In the first year of the pandemic, contact reduction was the only way to control infection rates. Governments around the world imposed school and business closures, work-from-home mandates, and travel restrictions. Less than a year later, vaccination emerged as the second major tool to curtail infection rates and allowed for a brief restoration of normalcy in countries such as Israel or Denmark. However, the continued evolution of SARS-COV2 might give rise to immune evasive variants which would nullify gains made through mass vaccination campaigns.
However, the unprecedented control that we hold over the progression of the pandemic means that we can reduce the probability of emergence of a vaccine resistant variant and its catastrophic consequences.
Which human decisions could limit the probability of emergence of vaccine resistant variants? In our paper, published in Nature Human Behaviour, we analyze the effect the two main variables that can be controlled by governmental policies and individual choices: (i) the number of new infections that occur each day and (ii) the number of people that are vaccinated each day. We have also explored several other variables that affect the evolution of vaccine resistance: the extent of vaccine hesitancy in a population, the launch of booster vaccination campaigns and the design of the vaccine itself.
What is the common point of policies that reduce the probability of emergence of vaccine resistance?
The simplicity of our finding is linked to a surprising observation which we made at the beginning of this project. After downloading infection rate data from six countries (Brazil, France, Germany, Israel, the United Kingdom and the United States), we plotted the reproductive coefficient of SARS-COV2 along time (see Figure 1). It had been oscillating around one for much of the pandemic. Simply put, this means that each infected individual has infected, on average, one other individual. Hence, the number of new infection cases per day has been oscillating around a constant value.
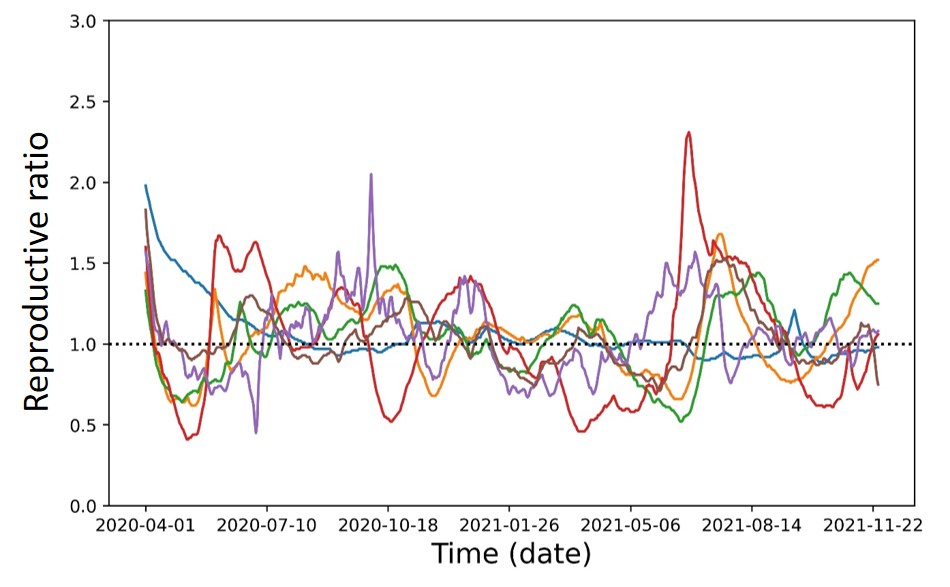
Figure 1: The reproductive ratio of SARS-COV2 in six countries (Brazil, France, Germany, Israel, United Kingdom and the United States) from the beginning of the pandemic to today. We notice that the reproductive ratio has been fluctuating around 1 due to the cycle of the tightening and loosening of social distancing measures. This observation allows us to derive a simple formula for the probability of vaccine resistance emergence.
Retrospectively, this observation is less surprising than it seemed. The COVID-19 pandemic has been characterized by an all-too-familiar cycle: first, the number of new infections rises such that the expected number of seriously ill patients exceeds the capacity of the healthcare system in a country or city. In response, governments impose contact reduction measures such as work-from-home mandates and school and business closures. After several weeks, the number of new infections declines, and governments release the lockdown. After a brief period of relaxation of measures for contact reduction, the number of new infections per day rises again.
From a mathematical point of view, a constant number of infections per day simplifies the analytical treatment of the probability for emergence of vaccine resistance. The total number of infections is the crucial determinant of this probability. Moreover, the speed of vaccination is important. Fast vaccination (of the entire eligible population) can prevent the emergence of resistance for infection rates that would otherwise give rise to almost certain evolution of vaccine resistant variants. Vaccination acts primarily by limiting the total number of infection cases.
How can we understand this conclusion? Each infection is an opportunity for the virus to mutate and acquire the genotype required for vaccine resistance. Hence, the probability that the vaccine resistant genotype has not emerged decreases exponentially with the number of infections. Limiting the number of infection cases is in the realm of possibilities of policy makers and could mean ending the pandemic if the emergence of resistant variants is indeed prevented.
Emergence of vaccine resistance and current events
The simplicity of our formula allows for the interpretation of current events in the light of the concern for emergence of vaccine resistance. Just in the week following the acceptance of our paper for publication, the new Omicron variant appeared in the headlines of world news.
The data about Omicron are still partial at the time of writing of this post. However, some encouraging studies indicate that Omicron could have a lower ability to infect lung cells, and therefore might be less likely to lead to serious complications. Surprisingly, the number of hospitalizations has not been strongly correlated with the number of cases in the beginning of the Omicron wave. This could be due to pre-existing population immunity from vaccination against the ancestral strain or a lower virulence of Omicron, or - most likely - a combination of both.
A major motivation of governments to impose contact reduction measures was to prevent the collapse of healthcare systems under the pressure of an excessive number of critical cases of COVID-19. Now, as the rate of complications from Omicron is much less than from previous variants, many governments have tolerated never-seen-before infection rates without imposing any restrictive measures.
The Omicron wave could have either an excellent or a catastrophic outcome. Due to its high infectiousness, many individuals who chose not to be immunized by vaccination will now become immunized by infection, potentially leading to herd immunity and thus the elimination of the virus. However, the high number of infection cases might also be an opportunity for fully vaccine resistant new variant to arise.
Follow the Topic
-
Nature Human Behaviour

Drawing from a broad spectrum of social, biological, health, and physical science disciplines, this journal publishes research of outstanding significance into any aspect of individual or collective human behaviour.





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in