How did they feel? A “Mental health check-up” with community-dwelling adults before and during COVID-19
Published in Public Health and Behavioural Sciences & Psychology
COVID-19 became a pandemic four years ago, and it was a stressful period for all. During that period of time, did you ever feel a little lonely about being unable to meet up with friends and family? Anxious about getting sick? Or even hopeless or doubtful that lives would return to what was “normal” again?
Well before the pandemic, older adults were already at greater risk of experiencing these thoughts and feelings than other age groups. For this reason, older adults tend to report greater challenges such as reduced mobility, social isolation, chronic illnesses, grief, and accessing healthcare services. With the pandemic, these existing challenges have become even more complex, as demonstrated by increased prevalence rates of loneliness, depression, and anxiety symptoms.
For many diseases, there is more than one clear and common cause. Would you say that a person developed diabetes only because of overeating sugar? Instead, it is more likely that a constellation of symptoms interacts with each other, such as lack of exercise, an unhealthy body weight, and genes. The same concept can be applied to mental health. Understanding how different mental health and psychiatric symptoms interact with each other (known as networks) can facilitate the development of more targeted interventions. Therefore, our research compared the networks of common risk factors and mental health problems (loneliness, depressive symptoms, and anxiety symptoms) in community-dwelling older Chinese people before and during a stressful event, COVID-19.
What did we find?
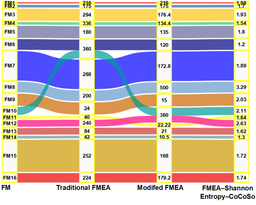
We recruited older adults (aged ≥ 60) at risk for depression through non-governmental organizations in Hong Kong. The data before COVID-19 was collected from 2016 to 2019 (n = 2549). The data during COVID-19 was collected from 2020 to 2023. In the COVID-19 pandemic, strict social distancing restrictions and quarantine measures were imposed (n = 3506). Through participants’ self-reported loneliness, depression and anxiety symptoms, we found that during the pandemic, the interactions between these symptoms were more complex and spread more easily than before the pandemic. In addition, being restless (an anxiety symptom) is the most critical symptom in the loneliness-depression-anxiety symptoms network both before and during COVID-19.
What are the implications?
The results suggested that although older adults’ external social interactions and networks were restricted during the pandemic, the network of their inner mental health problems widened. Specifically, the connections between feeling isolated from others (loneliness symptom), feeling worthless/guilty (depressive symptom), and feeling afraid as if something awful might happen (anxiety symptom) became stronger.
The study found that the association between centrality and symptom severity was unrelated in our sample of older adults. Although our sample of older adults reported the greatest feelings of loneliness, the key symptom in the loneliness-depression-anxiety network is, in fact, an anxiety symptom of being restless. What does this imply? There might be a discrepancy between symptom severity and the central symptom that plays a vital role in perpetuating the network. Feeling restless is also commonly reported by older people and often gets overlooked; in designing interventions to reduce or prevent loneliness, frontline mental health professionals may consider integrating ways to calm down restlessness.
Another meaningful connection that we have found was the strong association between suicidal ideation and feeling isolated during COVID-19. Social distancing measures to reduce virus spread may be at the expense of further heightening older adults’ feelings of isolation and loneliness. We suggest that promoting peer support and social interactions through social media or increasing access to telehealth services may be beneficial during public health crises.
More attention to high-risk groups
We directly compared the pre-COVID-19 loneliness-depression-anxiety symptoms network with the network during COVID-19 in the current sample. We found that older adults who were already at risk of depression pre-COVID-19 are more likely to experience more persistent symptoms during COVID-19, as the activation of one symptom could “spread the virus” onto another symptom. To mitigate this negative spiral, we suggest more attention to those at-risk groups and provide preventive care to target loneliness.
The way forward
By understanding the symptom network of loneliness, depression, and anxiety before and during COVID-19, our paper discusses essential implications for mental health service providers to develop more targeted interventions to promote older adults’ mental health. In this unprecedented era, you might be worried about other future mental health crises that may yet arise. The paper also provides suggestions to mental health professionals and policymakers to support the mental health of older adults better.
The current study focused only on older adults at risk of depression. Our main message here is not that those at risk are even more vulnerable in times of a global public health crisis. Instead, do not forget that we can become more resilient after a stressful encounter. We welcome other researchers and colleagues to further look into how the network of loneliness-anxiety-depression may have changed post-COVID-19. Maybe we all have developed a greater capacity to deal with stressors, as we all had a “mental health stress inoculation” over the past years.
Follow the Topic
-
Scientific Reports

An open access journal publishing original research from across all areas of the natural sciences, psychology, medicine and engineering.
Related Collections
With Collections, you can get published faster and increase your visibility.
Reproductive Health
Publishing Model: Hybrid
Deadline: Mar 30, 2026
Women’s Health
Publishing Model: Open Access
Deadline: Feb 28, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in