Incidence of COVID-19 diagnoses among smokers and smokeless tobacco users in a cohort study from Sweden
Published in Healthcare & Nursing
The recent (and still ongoing) pandemic due to SARS-CoV-2 and its variants obliged the scientific community to face several puzzling questions, not the least concerning pathways to infection and predictors of the clinical course. Why tremendous mortality was seen in some contexts and not in others? Why do (even healthy) men die more than women? Why were children relatively spared in the early stage of the pandemic?
Scientists were also taken aback by the role of tobacco smoking. Early alarming reports of smoking predicting an anticipated poor prognosis of the disease among hospital patients (1) were soon followed by repeated observations that smokers were indeed under-represented among patients requiring hospitalization compared with the underlying population (2). A long story had just begun.
In fact, reports of a lower risk of the disease among smokers increased in the following months, and a living review and meta-analysis supported a lower incidence of the disease among current compared with never-smokers (3).
But why would a tremendously hazardous exposure such as smoking entail a lower incidence of a viral disease which targets the respiratory system? The most obvious explanation would be that those getting tested, diagnosed, and treated are very different than those who are not (selection bias). If for instance smokers were less represented among individuals who are frequently tested for infection with SARS-CoV-2 this could explain the negative association. Since “being tested” is a wild card, as varying strategies have been employed in different contexts, this bias is hard to rule out. Also, smokers and non-smokers may differ as to the opportunity to be infected, or other characteristics affecting the disease severity.
Notwithstanding, hypotheses about a possible protective role of nicotine emerged (2). According to these hypotheses nicotine could play a “double agent” role, partly up-regulating the receptors for the SARS-CoV-2 virus in the airways (4); partly inhibiting the inflammatory response in the lungs (5). Some, but not all mechanistic studies offered some support to the “nicotine pathway”, but empirical evidence in humans is typically missing given the difficulty to conduct randomized experiments in this field. In the meantime, authoritative sources including the WHO (6) warned about premature conclusions and endorsed well conducted population studies.
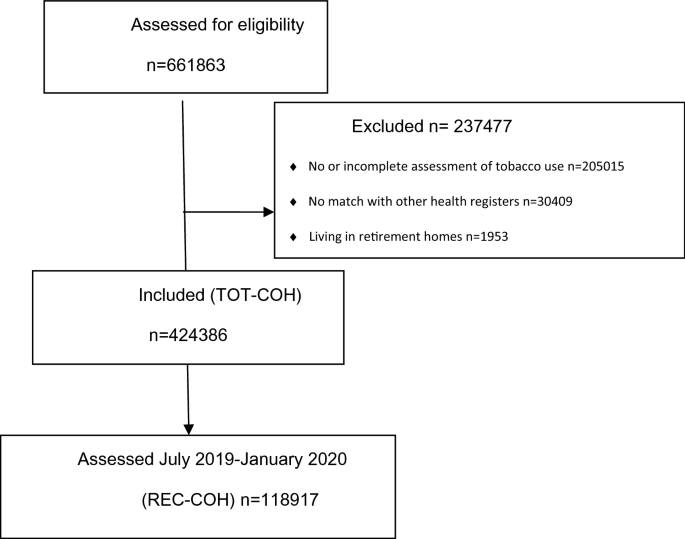
The idea for the study just published in Scientific Reports (7) was born in this climate, during the spring of 2020, due to inspiring discussions among public health epidemiologists based in the Stockholm regional health care and researchers at the Karolinska Institutet. We identified a unique dataset generated within the regional public dental health care, where current tobacco use is systematically assessed during preventive visits. This resulted in a sample of more than 400 thousand individuals with information on tobacco use, including both cigarette smoking and the use of Swedish moist oral tobacco known as snus.
In a next step this data was linked to computerized health care and demographic registers reporting diagnoses of COVID-19 and other information. Between February and October 2020 there were 6541 cases of verified cases of first-time infections with SARS-CoV-2 in this sample, of whom slightly more than 1400 required hospital admission.
A further step was undertaken when a scientific Consortium among three Nordic Countries was launched, to explore the same scientific question in population-based studies conducted in different contexts (8 ).
The newly published Swedish study (7) presents most of the desirable methodological characteristics advocated to minimize the risk of bias. The protocol of the study was preregistered. It includes a large population (not a clinical) sample. Tobacco use was assessed before the pandemic, thus avoiding the risk that concurrent behavioral changes would reverse the association. Several factors differing between tobacco users and non-users could be controlled for in the statistical analysis, among others occupational risk of infection, cohabitation with others and co-morbidity. Sensitivity analyses were conducted to triangulate the underlying question of a potential causal association between tobacco use and the risk of COVID-19.
Perhaps the most salient feature of the study was the information on snus, a type of tobacco delivering high doses of nicotine to the user, but without consequences for the respiratory system. If nicotine would play a role in the determinism of the lower risk observed among smokers the use of snus should appear as a similar or even more pronounced association.
We found no support for this association. Snus users (especially women) had a higher risk of receiving a diagnosis of COVID-19 than non-users of tobacco. A reduced risk of such diagnosis was apparent among current smokers.
Therefore, the data in this study did not support the hypothesis that nicotine would be beneficial towards the infection with SARS-CoV-2 or would improve the prognosis of COVID-19. The reason why smoking was associated with a decreased probability to receive a diagnosis of COVID-19 continues to be elusive.
Limitations of the study include the possibility of bias due to smokers being less likely and snus users more likely to be tested than non-users of tobacco; or to differences between tobacco users and non-users that we were not able to tease out (residual confounding); and the lack of information on past tobacco use. Therefore, the results should be weighed together with prior and ongoing studies.
Finally, some reflections on the implications of this and similar studies. Should the public health message about smoking be modified because of these results? Not at all. The overall consequences of smoking are deadly, and stopping smoking is beneficial to health, irrespective of whether the risk of a few diseases (such as endometrial cancer, or pre-eclampsia) (9) may be decreased among smokers.
So, why would this study be important? Because we believe that digging into paradoxes pushes scientific thinking beyond the obvious and opens for new insights on mechanisms of diseases.
References
- Liu, W. et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chinese medical journal 133, 1032 (2020)
- Farsalinos, K., Barbouni, A. & Niaura, R. Systematic review of the prevalence of current smoking among hospitalized COVID-19 patients in China: could nicotine be a therapeutic option? Internal and emergency medicine 15, 845-852 (2020)
- Simons, D., Shahab, L., Brown, J. & Perski, O. (2021). The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: A living rapid evidence review with Bayesian meta-analyses (version 12). Qeios. doi:10.32388/UJR2AW.15
- Russo P, et al. COVID-19 and smoking: is nicotine the hidden link? Eur Respir J. 4;55(6):2001116 (2020)
- Kloc M, Ghobrial RM, Kubiak JZ. How nicotine can inhibit cytokine storm in the lungs and prevent or lessen the severity of COVID-19 infection? Immunol Lett. 224:28-29 (2020)
- World Health Organization. Smoking and COVID-19. Available from: https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19, 2020
- Galanti MR. et al. Current tobacco use and COVID-19 diagnoses in a cohort of adult clients of public dental clinics in Sweden. Scientific Reports, 13:1204 (2023) doi: 1038/s41598-023-28091-4
- Peña S. et al. Tobacco use and risk of COVID-19 infection in the Finnish general Scientific Reports, 12(1):20335 (2022)
- Office of the Surgeon General (US); Office on Smoking and Health (US). The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2004.
Follow the Topic
-
Scientific Reports

An open access journal publishing original research from across all areas of the natural sciences, psychology, medicine and engineering.
Related Collections
With Collections, you can get published faster and increase your visibility.
Reproductive Health
Publishing Model: Hybrid
Deadline: Mar 30, 2026
Women’s Health
Publishing Model: Open Access
Deadline: Feb 28, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in