Insulin resistance with associated hyperinsulinemia, an independent risk factor for many diseases
Published in General & Internal Medicine and Public Health
A large scientific literature supports the concept that insulin resistance with associated hyperinsulinemia is closely related to the development of type 2 diabetes, cardiovascular disease, cellular senescence and cancer, degenerative diseases, and has been shown to be a condition associated with increased all-cause, cardiovascular disease and neoplasm mortality.
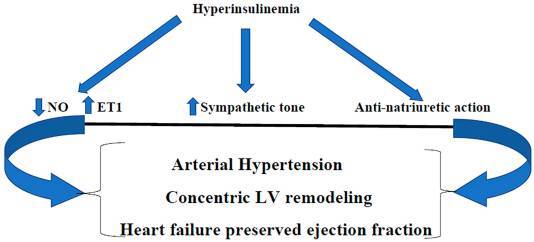
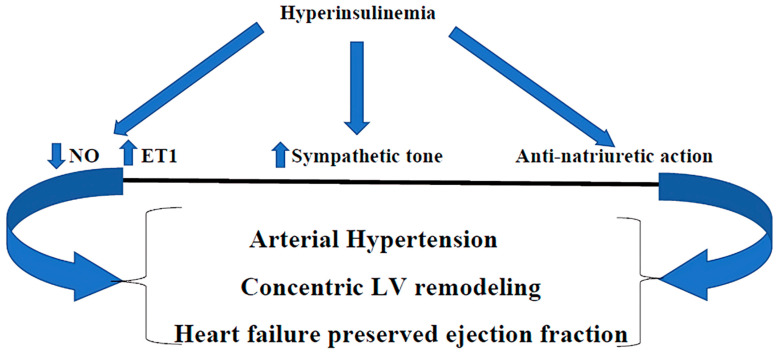
The prevalence of insulin resistance has been progressively increasing for several years, as has, consequently, type 2 diabetes. Insulin resistance is a pathological condition that precedes the onset of type 2 diabetes by many years (even up to 15 years) and over the years produces significant alterations at the cardiovascular and non-cardiovascular level, so much so that, if we investigate a patient with recently onset type 2 diabetes, we already find many alterations, so much so that the diabetic patient is, by guidelines, treated as a subject who has already had a cardiovascular event. As mentioned, insulin resistance is characteristically associated with chronically higher levels of circulating insulin, particularly in the postprandial period when foods rich in carbohydrates have been consumed. Insulin is a hormone and like all hormones it causes harm whether both its levels are low and chronically increased. There is considerable scientific literature that explains how increased levels of insulin can cause harm. For example, hyperinsulinemia determines an alteration of vascular homeostasis towards vasoconstriction, due to an altered equilibrium between nitric oxide (NO) and endothelin-1 (ET-1), clearly in favor of the latter. Furthermore, it determines activation of the sympathetic system with an increase in circulating norepinephrine and, through its receptors in the renal tubules, increases sodium reabsorption. This is probably the basis of what we have called for many years “essential arterial hypertension”(Figure 1). Furthermore, chronic hyperinsulinemia, producing cardiac remodeling, can determine heart failure with preserved ejection fraction (HFpEF).
Figure 1. Hyperinsulinemia, through the imbalance between NO and ET1 (in favor of the latter), the stimulation of sympathetic tone, and the anti-natriuretic action, produces arterial hypertension, concentric LV remodeling, and heart failure with preserved ejection fraction. NO: nitric oxide; endothelin-1; LV: left ventricle.  : Decreased;
: Decreased;  : Increased.
: Increased.
But, being also a growth factor, it also produces many other alterations. And what do we do? We do not intervene on it promptly but, most of the times, we wait for the development of diabetes to intervene. We intervene, therefore, too late!
Follow the Topic
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcement
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
It seems to me very logical, as much as that, early diagnosis and prompt intervetion could preserve the normal heart function, prevent the development of Diabetes and all the following metabolic disorders secondary to hyperinsulinemia. The most important interventions could be change of lifestyle, exercise and continuous screening.