Insulin resistance with associated hyperinsulinemia as cause of essential arterial hypertension
Published in Biomedical Research
Essential (primary) hypertension is so called because it has no known triggers, unlike secondary hypertension, which is mostly caused by renal, endocrine, and vascular damage. Essential hypertension is highly prevalent, accounting for about 90% of all forms of hypertension. For this reason, we treat this form of hypertension without knowing its cause.
The classes of drugs used to treat hypertension are sufficiently effective, but since they do not directly target the cause of hypertension, they often do not completely control it. In addition, these drugs, like other drugs used in chronic therapies, often cause side effects that undermine patient compliance.
Essential hypertension is very frequently associated with overweight, obesity, particularly visceral obesity, and metabolic syndrome, all conditions associated with insulin resistance. It should be noted that essential hypertension and insulin resistance have a comparable prevalence in the adult population, i.e., around 30-35%. Insulin resistance associated with hyperinsulinemia, in addition to being the main determinant of type 2 diabetes, causes multiple negative effects on our body.
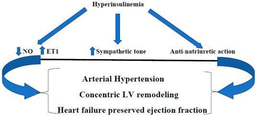
Among other things, hyperinsulinemia, which is an important and constant feature of insulin resistance, causes high blood pressure through numerous proven mechanisms: 1. Increased secretion of endothelin-1 (ET-1) at the vascular level and, conversely, reduction in the secretion of nitric oxide (NO), resulting in endothelial dysfunction and vasoconstriction [1-3]; 2. Increased secretion of norepinephrine, another hormone with vasoconstrictive action [4, 5]; 3. Increased tubular reabsorption of sodium and water , leading to an expansion of blood volume [6, 7]; 4. Advanced glycation end products are increased in insulin resistance and are related to a rise in vascular stiffness in hypertensive patients [8]; 5. Insulin resistance with associated hyperinsulinemia can directly stimulate components of the RAAS [9, 10].
It is therefore clear from the above that the majority of cases of essential hypertension can be attributed to hypertension caused by insulin resistance. Recognizing insulin resistance as the cause of essential hypertension would change the approach to treating it, because once the cause has been identified, it would no longer be considered essential hypertension, but rather secondary hypertension caused by an endocrine disorder (hyperinsulinemia). Furthermore, the therapy should be aimed primarily at counteracting insulin resistance, which would probably result in better blood pressure control with lower doses of antihypertensive drugs, improving the outcomes and reducing health care spending. I believe that it is now time to change the name from essential hypertension to insulin resistance hypertension for these forms of hypertension.
References
- Fazio, S.; Bellavite, P.; Affuso, F. Chronically Increased Levels of Circulating Insulin Secondary to Insulin Resistance: A Silent Killer. Biomedicines. 2024 Oct 21;12(10):2416. doi: 10.3390/biomedicines12102416. PMID: 39457728; PMCID: PMC11505545.
- Fazio, S.; Affuso, F.; Cesaro, A.; Tibullo, L.; Fazio, V.; Calabrò, P. Insulin Resistance/Hyperinsulinemia as an Independent Risk Factor That Has Been Overlooked for Too Long. Biomedicines. 2024 Jun 26;12(7):1417. doi: 10.3390/biomedicines12071417. PMID: 39061991; PMCID: PMC11274573.
- Potenza, M.A.; Marasciulo, F.L.; Chieppa, D.M.; Brigiani, G.S.; Formoso, G.; Quon, M.J.; Montagnani, M. Insulin resistance in spontaneously hypertensive rats is associated with endothelial dysfunction characterized by imbalance between NO and ET-1 production. Am J Physiol Heart Circ Physiol. 2005 Aug;289(2):H813-22. doi: 10.1152/ajpheart.00092.2005. Epub 2005 Mar 25. PMID: 15792994.
- Zamami, Y.; Takatori, S.; Yamawaki, K.; Miyashita, S.; Mio, M.; Kitamura, Y.; Kawasaki, H. Acute hyperglycemia and hyperinsulinemia enhance adrenergic vasoconstriction and decrease calcitonin gene-related peptide-containing nerve-mediated vasodilation in pithed rats. Hypertens Res. 2008 May;31(5):1033-44. doi: 10.1291/hypres.31.1033. PMID: 18712059.
- Arauz-Pacheco, C.; Lender, D.; Snell, P.G.; Huet, B.; Ramirez, L.C.; Breen, L.; et al. Relationship between insulin sensitivity, hyperinsulinemia, and insulin-mediated sympathetic activation in normotensive and hypertensive subjects. Am J Hypertens. 1996 Dec;9(12 Pt 1):1172-8. doi: 10.1016/S0895-7061(96)00256-7. PMID: 8972887.
- Semplicini, A.; Ceolotto, G.; Massimino, M.; Valle, R.; Serena, L.; De Toni, R. et al. Interactions between insulin and sodium homeostasis in essential hypertension. Am J Med Sci. 1994 Feb;307 Suppl 1:S43-6. PMID: 8141164.
- Nizar, J.M.; Shepard, B.D.; Vo, V.T.; Bhalla, V. Renal tubule insulin receptor modestly promotes elevated blood pressure and markedly stimulates glucose reabsorption. JCI Insight. 2018 Aug 23;3(16):e95107. doi: 10.1172/jci.insight.95107. PMID: 30135311; PMCID: PMC6141164.
- McNulty, M.; Mahmud, A.; Feely, J. Advanced glycation end-products and arterial stiffness in hypertension. Am J Hypertens. 2007 Mar;20(3):242-7. doi: 10.1016/j.amjhyper.2006.08.009. PMID: 17324733.
- Thethi T, Kamiyama M, Kobori H. The link between the renin-angiotensin-aldosterone system and renal injury in obesity and the metabolic syndrome. Curr Hypertens Rep. 2012 Apr;14(2):160-9. doi: 10.1007/s11906-012-0245-z. PMID: 22302531; PMCID: PMC3337881.
- Luther, J.M.; Brown, .NJ. The renin-angiotensin-aldosterone system and glucose homeostasis. Trends Pharmacol Sci. 2011 Dec;32(12):734-9. doi: 10.1016/j.tips.2011.07.006. Epub 2011 Aug 29. PMID: 21880378; PMCID: PMC3223326.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in