Invasive lobular carcinoma (ILC) is the most common special subtype of breast carcinoma. In contrast to carcinoma of no special type (NST, also known as invasive ductal carcinoma or IDC), ILC lacks duct formation and characteristically shows single cell infiltrative growth pattern which is the results of biallelic inactivation of the CDH1 gene (codes for E-cadherin). ILC has been reported to show some unique clinical features compared to IDC. ILC forms a poorly defined mass and the tumor size is often underestimated on clinical exam and imaging. It is questionable whether the prognosis of ILC is better, similar, or worse than grade and stage-matched IDC. However, the pattern of metastasis is unique to ILC with more frequent metastasis to visceral organs such as gastrointestinal tract, uterus, and ovaries. ILC shows minimal response to neoadjuvant chemotherapy compared to IDC, but this relative resistance to cytotoxic chemotherapy is likely due to receptor profile and proliferation (high receptor expression levels and lower proliferation in ILC) rather than due to the histological pattern itself.
A diagnosis of ILC can be confirmed using immunohistochemical staining for E-cadherin which frequently shows loss of reactivity in the tumor cells. At the current time, the world health organization (WHO) classification of tumors, 5th edition does not recommend performing E-cadherin immunohistochemical staining for breast tumor classification but the reality is that 50% of the institutions do use it in a variety of ways. If E-cadherin IHC is not routinely used, then there is a potential to misclassify tumors, promotes use of non-standard terminology and significant inter-observer variability. Prior studies have also shown that subtyping of breast cancer as ILC achieves almost perfect agreement with a pre‐defined reference standard, if assessment is supported by E‐cadherin IHC.1 However, if E-cadherin is routinely performed but not appropriately optimized and validated, then again the tumors can be misclassified. Moreover, if the pathologists are unaware of “aberrant” reactivity of E-cadherin, tumors will still be misclassified. Absence of circumferential membranous E-cadherin reactivity should be classified as “aberrant” as it often correlates with CDH1 gene mutations (Figure 1).
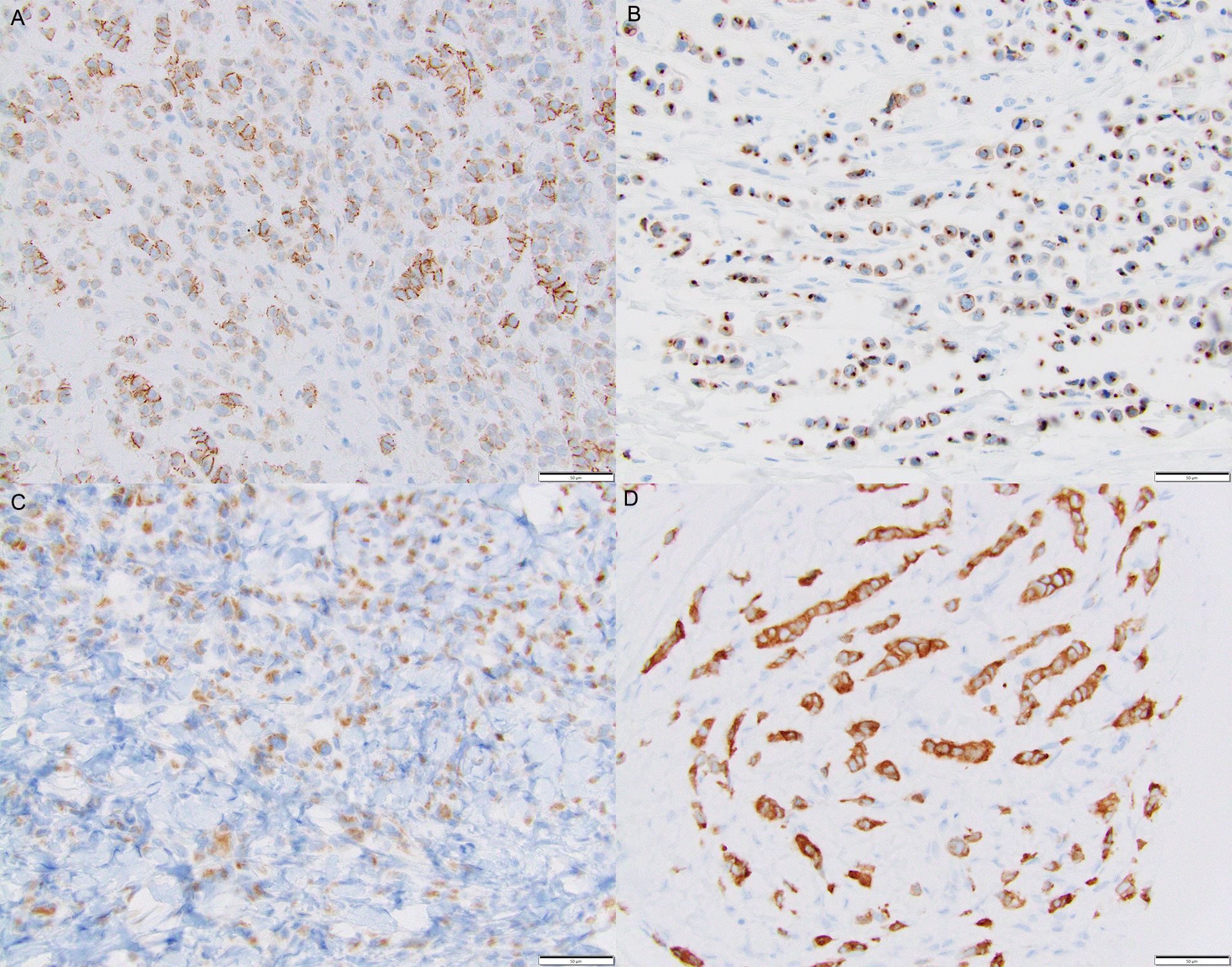
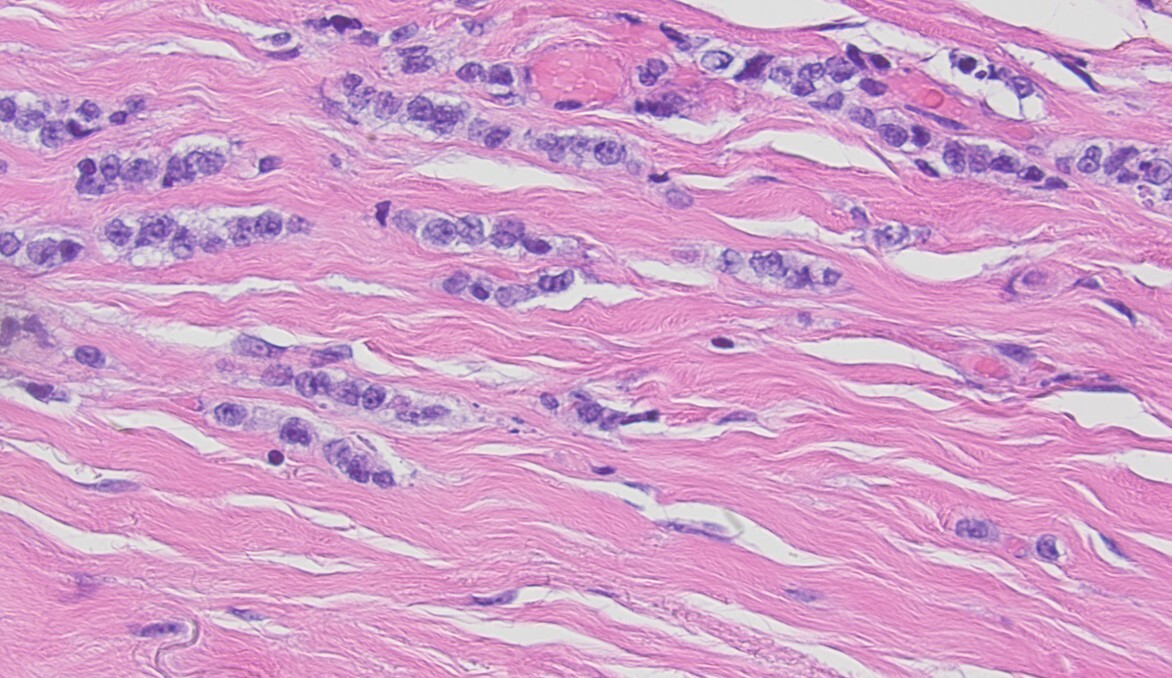
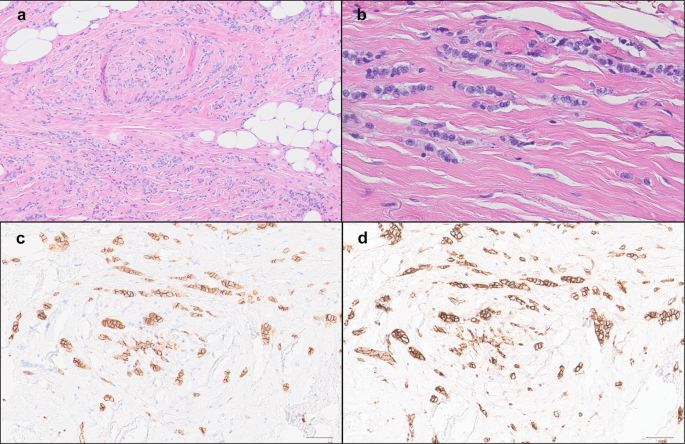
To improve standardization of ILC diagnosis, we have been routinely performing E-cadherin to confirm first time ILC diagnosis at our institution since 2004-2005. However, in doing so routinely, we have encountered tumors that morphologically resemble ILC on hematoxylin and eosin (H&E) stain slides but demonstrate circumferential membranous reactivity for E-cadherin. We have always wondered if these tumors follow a clinical course similar to ILC or IDC and whether they demonstrate characteristic CDH1 mutations. We labeled these tumors lobular-like invasive mammary carcinoma (LLIMCa or LiMCa) for our study and compared and contrasted their clinical-pathologic features with grade matched IDC and ILC. We also performed an exploratory molecular analysis of 7 LiMCa and 7 ILC to understand the molecular mechanisms that results in this morpho-immunohistologic appearance.
The clinical-pathologic features of LiMCa appears to be intermediate between IDC and ILC. LiMCa shared some features with IDC (such as frequency of lympho-vascular space invasion), and some features with ILC (underestimation of tumor size on imaging). There doesn’t appear to be a difference in clinical outcome based on histologic subtype (ILC, IDC, or LiMCa). The prognostic markers that are significant for other breast tumor types are also significant for LiMCa, i.e. better prognosis of lower pT and pN stage tumors. Interestingly, the multi-variable prognostic model, Magee Equation 2 was prognostic regardless of the tumor histology.
Our exploratory molecular analysis revealed interesting results. All examined ILC cases showed characteristic CDH1 mutations (frameshift indel and splice site mutations) coupled with loss of heterozygosity (LOH) of 16q locus consistent with prior published studies. LiMCa cases showed LOH of 16q but lacked the characteristic loss of function mutations of the CDH1 gene. Four of 6 cases tested showed CDH1 promoter methylation but two cases (with intense circumferential E-cadherin and p120 staining) were negative even for CDH1 promoter methylation. The morphologic discohesion of cells in LiMCa could partly be explained by CDH1 promoter methylation in some, but not all cases. Future studies may require whole genome sequencing to determine if the morphologic discohesion seen in LiMCa cases is driven by genetic inactivation of other genes playing key roles in epithelial cell-cell adhesion.
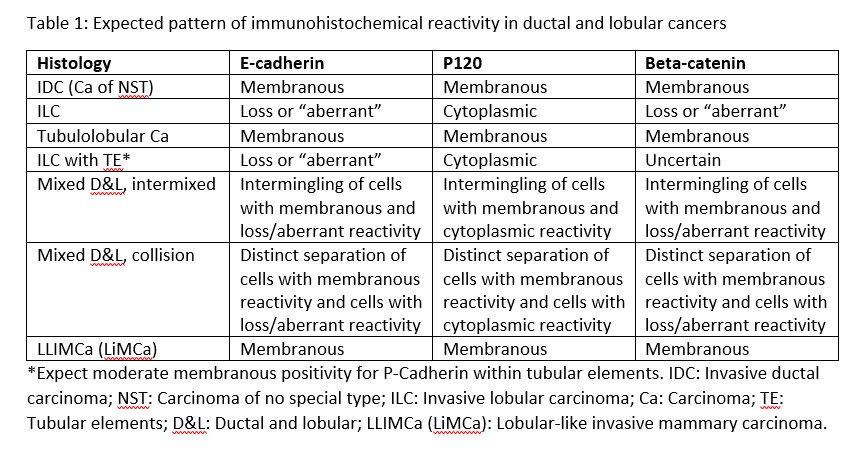
Our study further clarifies the terminology used in describing breast carcinomas with ambiguous morphology (ductal versus lobular) and classification based on E-cadherin, and other cadherin-catenin junction protein like p120 and beta-catenin staining (Table 1).2 LiMCa appears to be distinct from the other described subtypes. Even after using numerous immunohistochemical stains for classification, some tumors are still difficult to categorize and it is reasonable to label them as invasive mammary carcinoma with indeterminate differentiation (ductal versus lobular). Targeted sequencing, CDH1 promoter methylation and in rare cases whole genome sequencing of such cases can provide further insight.
In summary, we describe the clinical-pathological features of LiMCa – a low to intermediate grade mammary carcinoma that shows single cell infiltrating growth pattern (like classical-type lobular carcinoma) but shows retained membranous expression of E-cadherin and other related proteins (p120 and beta-catenin). These tumors lack the characteristic CDH1 mutations but a proportion of them show CDH1 promoter methylation. Their clinical-pathological features are intermediate between ILC and IDC. The prognosis is related to tumor stage and multivariable prognostic model of Magee Equation score.3 Using LiMCa terminology will help us learn more about these peculiar tumors.
For more details, please see our publication.
Follow the Topic
-
npj Breast Cancer

This journal publishes original research articles, reviews, brief communications, matters arising, meeting reports and hypothesis generating observations which could be unexplained or preliminary findings from experiments, novel ideas or the framing of new questions that need to be solved.
Related Collections
With Collections, you can get published faster and increase your visibility.
Molecular Tumor Board in Breast Cancer
Publishing Model: Open Access
Deadline: Jul 22, 2026
Rare breast cancer subtypes
Publishing Model: Open Access
Deadline: Mar 24, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in