Tuberculosis (TB) remains a significant global public health challenge and is the largest cause of infectious disease death globally. Poverty and undernutrition are strongly linked to TB burden, and low-middle income countries (LMICs), such as India, suffer a greater global proportion of TB incidence and mortality. Unfortunately, efforts to reduce the TB burden can be hampered by events impacting the global food system, including, in more recent times, infectious disease pandemics and international wars which can cause changes to energy prices and restrictions to exports. Clark and colleagues from the London School of Hygiene and Tropical Medicine used mathematical modelling to predict and simulate the changes in TB incidence and mortality in India as a consequence of nutritional shocks to the food system generated from such global events.
What inspired the study?
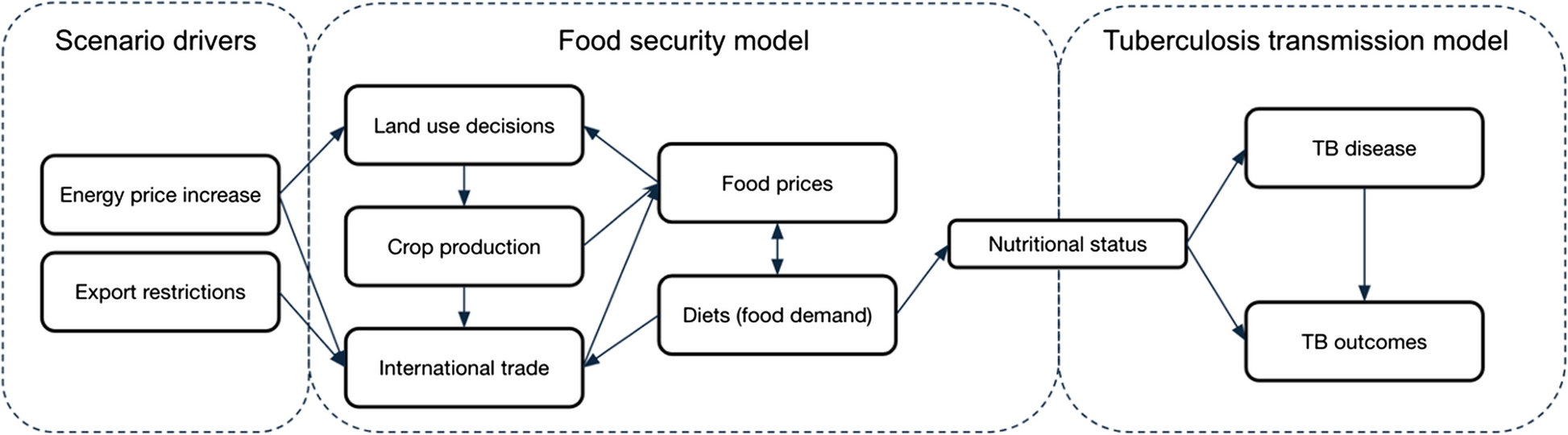
The World Health Organisation (WHO) developed an End TB Strategy that aims to reduce TB incidence by 80%, TB deaths by 90%, and to eliminate catastrophic costs for TB-affected households by 2030 [1]. Currently, most countries are not on track to meet these goals. A small, but not insignificant factor contributing to this may be nutritional shocks to the global food system from indirect environmental and social events. These often distal nutritional shocks can have rippling effects and ramifications on TB incidence and mortality, by increasing the proportion of the population with undernutrition, leading to an increase in the risk of developing TB. [2,3] The authors used a TB infection transmission model coupled with the LandSyMM food system model [4] to estimate the consequences of such nutritional shocks on the burden of TB to highlight their impact and the importance of considering additional preventative measures to reduce the TB burden.
Why is it important?
The findings help policy-makers and researchers to better appreciate that the impact of external, uncontrollable factors (for example, changes in energy prices and export restrictions resulting from external events such as global pandemics or war) can be wide reaching. In the case of TB, it is important to consider how impacts on food systems may influence undernutrition in a population, and the need for additional interventions to prevent the negative consequences. Importantly, in the worst-case scenario where the nutritional shock to the global food system is more severe (as modelled by Clark et al), the consequences on TB-related incidence and mortality in India could be significant over the next decade.
Did this study show anything unexpected?
Model estimates demonstrated that the TB burden may be influenced by nutritional shocks from environmental and social events. The impact of nutritional shocks on the TB burden is perhaps not unexpected, yet the authors empirical approach to the question has revealed alarming consequences. The findings indicated that nutritional shocks in the worst-case scenario, with both increases in energy prices and export restrictions, could increase the TB incidence and mortality rates by 5.0% and 4.9%, respectively, in India in 2035, and lead to an additional 1.1 million TB episodes and 177.5 thousand deaths between 2022–2035.
What is the wider significance of the study findings?
These findings highlight the importance of worldwide interactions and cascading risks on food security, which potentially have detrimental influences on attempts to end TB in India and globally through increasing undernutrition. The authors indicate that the impact of crises on TB may be underappreciated if the impact on nutrition is not considered. The implications are significant for guiding future research efforts and for informing policy makers in high TB burden countries about the importance of nutritional shocks when monitoring TB incidence and mortality.
References:
World Health Organization. WHO | WHO End TB Strategy. 2015.
World Health Organization. Global tuberculosis report. 2024.
Bhargava A, et al. Attributable is preventable: corrected and revised estimates of population attributable fraction of TB related to under-nutrition in 30 high TB burden countries. J Clin Tuberc Mycobact Dis.2022;27:100309.
Landsymm. https://landsymm.earth/. Accessed 19 Dec 2023.
Follow the Topic
-
BMC Global and Public Health

An open access, transparent peer review journal publishing outstanding and influential research and opinion of broad interest to all professional communities involved in global and public health research, policy-making, implementation and delivery worldwide.
Related Collections
With Collections, you can get published faster and increase your visibility.
Understanding the HIV care continuum: Progress and challenges
BMC Global and Public Health is calling for submissions to our Collection on understanding the complexities and advancements in global health frameworks. This Collection will highlight key findings and challenges in maintaining continuity of care for populations affected by HIV across diverse regions.
This Collection aims to explore the multifaceted nature of HIV care, examining the ongoing challenges and recent advances in care delivery systems. We welcome contributions that offer a comprehensive understanding of how access to care, quality of treatment, and sustained engagement with healthcare systems impact health outcomes for individuals living with HIV.
Potential topics include but are not limited to:
The role of diagnosis and early detection in improving long-term health outcomes
Strategies for improving linkage to care and retention in care
The impact of antiretroviral therapy in managing HIV
Barriers to viral suppression and achieving optimal care continuity
Innovations in pre-exposure prophylaxis (PrEP) for at-risk populations
The influence of socioeconomic, cultural, and political factors on HIV care accessibility
This Collection aims to contribute to a more thorough and collaborative understanding of HIV care challenges worldwide, focusing on solutions and the pathways needed to support people living with HIV, ensuring their access to effective, ongoing care. We look forward to receiving innovative and impactful research that will push the boundaries of our current knowledge.
We encourage work from local, regional, national, and global partnerships and collaboration among multidisciplinary scientists using multiple methodologies. We ask that authors be careful to use non-stigmatizing/preferred language in their manuscripts as outlined in relevant language guidelines for their respective fields.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Mar 18, 2026
Food security, nutrition, and dietary trends
BMC Global and Public Health is calling for submissions to our Collection on food security, nutrition, and dietary trends. These are interconnected elements that profoundly impact global health and well-being. As the world grapples with rapid population growth, climate change, and economic disparities, the challenges surrounding food access, quality, and sustainability have intensified. This Collection aims to gather diverse research that examines these complex relationships, focusing on how dietary patterns, food availability, and nutritional status influence overall health outcomes. By exploring the multifaceted nature of food systems, this Collection seeks to showcase pathways to achieve improved food security and nutritional health worldwide.
The goal of this Collection is to build a comprehensive body of knowledge that informs policy and practice. We encourage submissions that investigate:
Impact of dietary patterns on health outcomes
Addressing food insecurity through policy
Role of ultra-processed foods in nutrition
Personalized nutrition and dietary therapy
Nutritional supplements for malnutrition
This Collection supports and amplifies research related to SDG 2: Zero Hunger and SDG 3: Good Health and Well-Being.
We encourage work from local, regional, national, and global partnerships and collaboration among multidisciplinary scientists using multiple methodologies. We ask that authors be careful to use non-stigmatizing/preferred language in their manuscripts as outlined in relevant language guidelines for their respective fields.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: May 28, 2026
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in