
Explore the Research
Adiposity, metabolites, and colorectal cancer risk: Mendelian randomization study
Obesity is viewed as a likely cause of colorectal cancer (CRC, also known as bowel cancer) [1], but still unclear is whether risk differs for men and women, and exactly how obesity biologically causes CRC. Using a sort of naturally occurring trial called Mendelian randomization [2], which uses genetic information to better understand causality of modifiable factors, we examined whether two different measures of obesity – namely body mass index (BMI) and waist-hip-ratio (WHR) were associated with CRC risk among men and women separately. We also investigated whether circulating metabolites, or small molecules in blood which capture metabolic processes, could explain these relationships [3]. These Mendelian randomization methods, when key assumptions are met, help to minimise issues of confounding and reverse causation which are common pitfalls of observational studies [2].
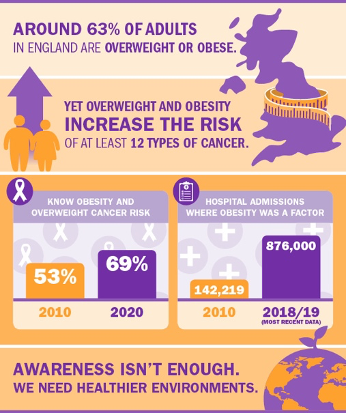
Obesity is viewed as an important risk factor for cancer by the World Cancer Research Fund (WCRF) https://www.wcrf-uk.org/uk/our-research/research-we-fund
As part of a collaboration between the International Agency for Research and Cancer (IARC) in France, the Fred Hutchinson Cancer Research Centre in the US, and the University of Bristol in the UK, we acquired summary statistics from three major consortia, including the Genetics of Epidemiology of Colorectal Cancer Consortium (GECCO), together describing the genotypes of over 100,000 individuals from 72 studies to better estimate the role of adiposity in CRC, separately by sex and anatomical sub-site (colon, proximal colon, distal colon and rectum). We used publicly available summary statistics describing the genetics of adiposity (BMI, WHR) and metabolites detected by targeted NMR spectroscopy. These metabolites included detailed lipid traits plus amino acids, fatty acids and inflammatory glycoproteins.
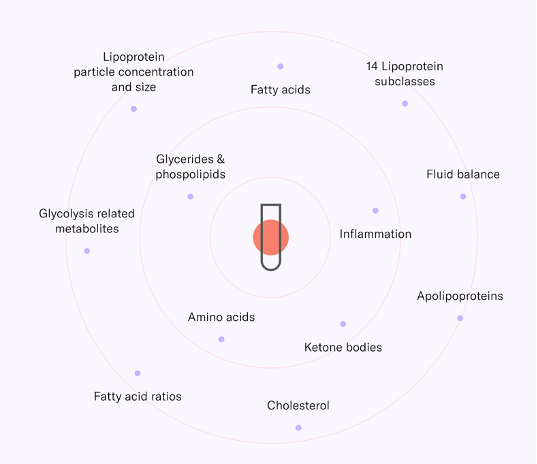
Metabolites detectable in blood using the Nightingale Health NMR panel https://nightingalehealth.com/research/blood-biomarker-analysis
Our results suggest that BMI and WHR associations do not differ substantially by CRC site, but do differ substantially by sex. Higher BMI is more strongly associated with CRC risk in men, whereas higher WHR is more strongly associated with CRC in women. This was surprising as BMI and WHR are highly correlated, and we hypothesise that this could be because women are more likely to store fat peripherally, meaning that WHR is better able to capture the extremes of adiposity in women.
A two-minute primer on Mendelian randomization
We explored potential mechanisms through which adiposity could influence CRC by examining metabolites as intermediate biomarkers. Despite examining over 100 metabolites from multiple biological subclasses, we did not identify any convincing metabolite-CRC associations which could explain the adipose-CRC relationship. Future studies using new and improved methodological techniques and exploring even more detailed metabolites, proteins, hormones, and inflammatory factors as potential mediators are needed to uncover the biological pathways between adiposity and CRC. This should be done among men and women separately given their markedly different risks from obesity. Understanding these pathways is more important than ever because of how common overweight and obesity are, and how difficult they are to reverse.
Read the paper here: https://rdcu.be/cclz2
References
- World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report. Diet, nutrition, physical activity and colorectal cancer. 2018.
- Davey Smith G, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003; 32(1): 1–22.
-
Bull CJ, Bell JA, Murphy N, et al. Adiposity, metabolites, and colorectal cancer risk: Mendelian randomization study. BMC Med. 2020; 18(1): 396.
Follow the Topic
-
BMC Medicine

This journal publishes outstanding and influential research in all areas of clinical practice, translational medicine, medical and health advances, public health, global health, policy, and general topics of interest to the biomedical and sociomedical professional communities.
Related Collections
With Collections, you can get published faster and increase your visibility.
Weight loss interventions and their health impacts
BMC Medicine is calling for submissions to our new Collection on weight loss interventions and their health impacts, emphasizing a variety of strategies, including dietary changes, physical activity, pharmacological treatments, and surgical options. We encourage submissions that explore the long-term effects of these interventions, adherence challenges, and strategies to address health inequities. The goal is to advance understanding and improve outcomes in weight management and overall health.
Weight loss interventions encompass a wide range of strategies aimed at reducing body weight and improving health outcomes. These interventions can include dietary changes, increased physical activity, pharmacological treatments, and surgical options such as bariatric surgery. As the global prevalence of obesity and related comorbidities continues to rise, understanding the efficacy and mechanisms of various weight loss interventions becomes increasingly crucial for public health. This Collection seeks to explore the diverse methodologies and outcomes associated with weight loss interventions, offering insights into their impacts on both individual and population health.
The significance of this research is underscored by the growing body of evidence linking obesity to numerous chronic health conditions, including diabetes, cardiovascular diseases, and certain types of cancer. Advances in pharmacological treatments, such as SGLT2 inhibitors and GLP-1 agonists, have emerged as promising options for weight management, demonstrating not only weight loss but also improved metabolic health. There are, however, challenges and limitations related to drug availability, healthcare delivery, and long-term treatment adherence with rapid weight gain when stopping treatment. Additionally, integrating behavioral strategies with nutritional and physical activity interventions has shown potential in enhancing adherence and long-term success. By further investigating these modalities, we can develop comprehensive approaches that address the multifactorial nature of obesity.
Continued research in this domain may yield innovative strategies that harness technology, such as mobile health applications and telehealth, to support weight loss interventions. As we deepen our understanding of the genetic, environmental, and behavioral factors influencing obesity, personalized interventions tailored to individual needs could emerge. This progress may lead to improved health outcomes, reduced health inequities, and ultimately a shift in the paradigm of obesity treatment and prevention.
We are looking for original manuscripts on topics including, but not limited to:
•Clinical trials investigating interventions for weight loss to promote health
•Real-world data on long-term effects and challenges of weight loss interventions
•Factors affecting long-term adherence to weight-loss or weight maintenance interventions
•Challenges and inequities in access to weight loss interventions
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being.
Publishing Model: Open Access
Deadline: May 07, 2026
Climate change and human health
BMC Medicine is calling for submissions to our new Collection on the health impacts of climate change. The relationship between global warming and human health is increasingly becoming a focal point in public health research. Rising temperatures, shifting weather patterns, and extreme weather events are projected to have profound effects on various health outcomes. From increased prevalence of vector-borne diseases to heightened risks of heat-related illnesses, the health implications of climate change are vast and multifaceted. This Collection aims to explore the direct and indirect impacts of global warming on health, examining how these changes affect vulnerable populations and health systems worldwide.
Understanding the implications of global warming for human health is crucial for developing effective public health strategies and interventions. Recent research has highlighted the links between climate change and a variety of health issues, including air pollution, water-borne diseases, and undernutrition. Advances in climate modeling and epidemiological studies have enhanced our ability to predict health outcomes related to climate change, providing invaluable insights that can inform policy decisions and health care planning.
Continued research in this area may lead to innovative solutions to mitigate the health impacts of climate change. For example, interdisciplinary approaches that integrate climate science, public health, and social determinants of health could reveal new pathways for adaptation and resilience. Future studies may also focus on the development of health infrastructure designed to withstand climate-related stresses, thus improving community health outcomes in an era of global warming.
We are considering manuscripts on, but not limited to the following topics:
-Impact of air pollution on health
-Heat-related illnesses
-Water-, and vector-borne diseases in a warming world
-Social determinants of health and climate vulnerability
-How health systems and infrastructure may be affected by climate change
-Nutrition and health in the context of climate change
-Impacts of climate change on non-communicable diseases
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 13 (Climate Action).
Publishing Model: Open Access
Deadline: Mar 02, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in