Personalizing Type 2 Diabetes Risk with Multimodal Data
Published in Healthcare & Nursing, Bioengineering & Biotechnology, and General & Internal Medicine
Type 2 diabetes: a complex challenge
Type 2 diabetes (T2D) affects hundreds of millions of people worldwide, yet preventing its onset and complications remains a major challenge. One reason for this difficulty lies in the complex nature of T2D, emerging from a mix of genetic, metabolic, behavioral, and environmental factors. Despite this complexity, current diagnostic tools like the HbA1c and fasting glucose tests offer only a limited snapshot of a person’s metabolic health.
We believed a broader, more holistic view, integrating diverse types of data, was needed to uncover more personalized insights into diabetes risk.
A new kind of clinical study
To explore this, we launched the PRediction Of Glycemic RESponse Study (PROGRESS) with the goal of collecting real-world health data outside the traditional clinic setting. We enrolled 1,137 adults in the United States, comprising individuals diagnosed with prediabetes or T2D, as well as metabolically healthy participants.
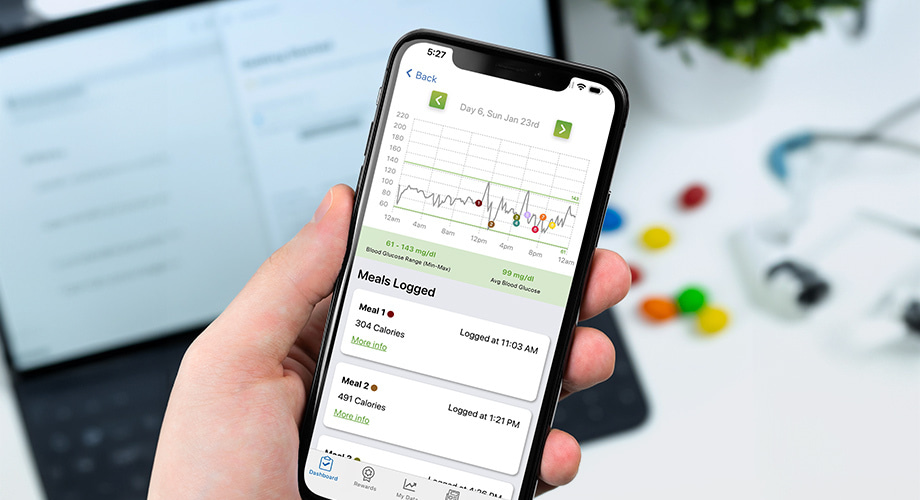
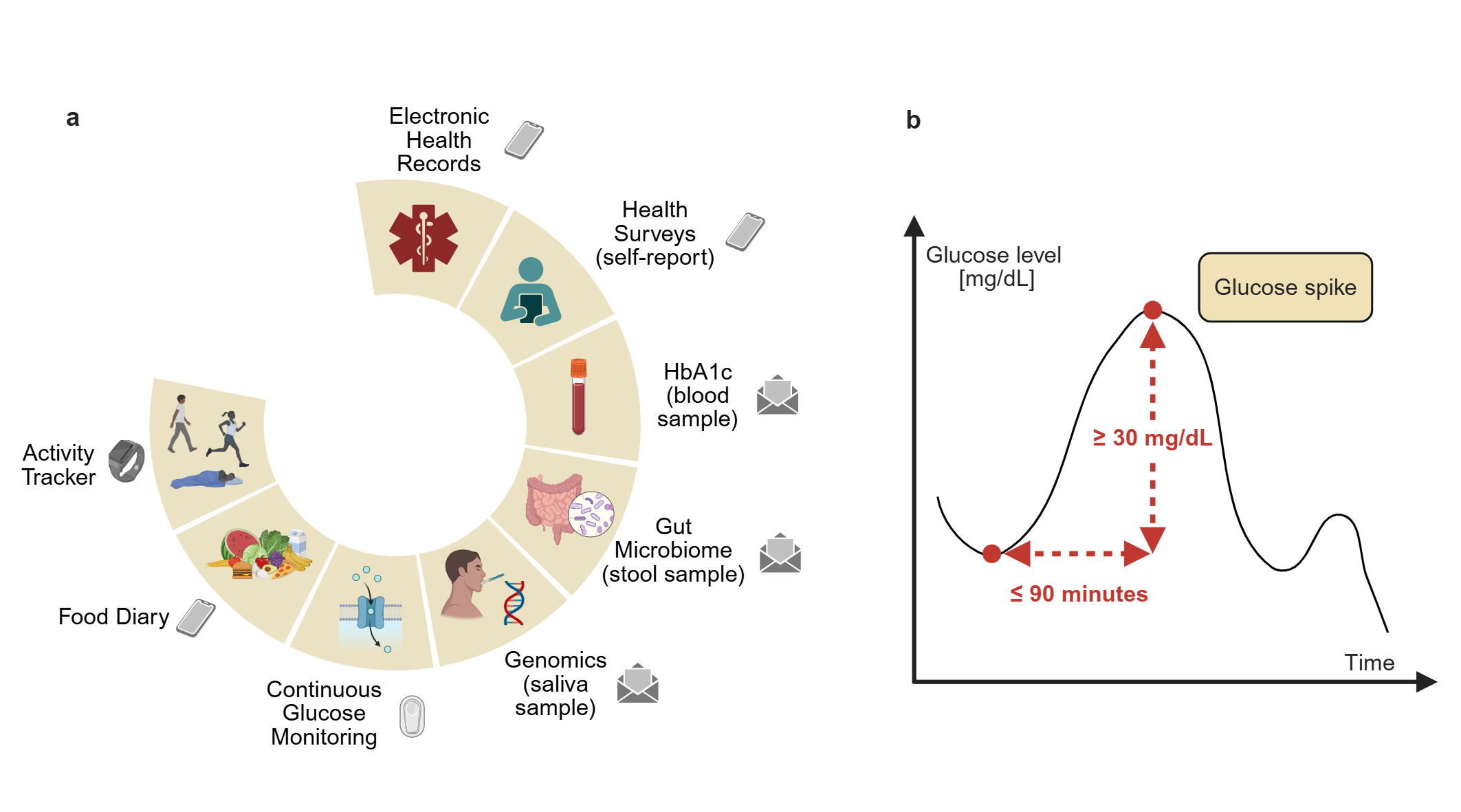
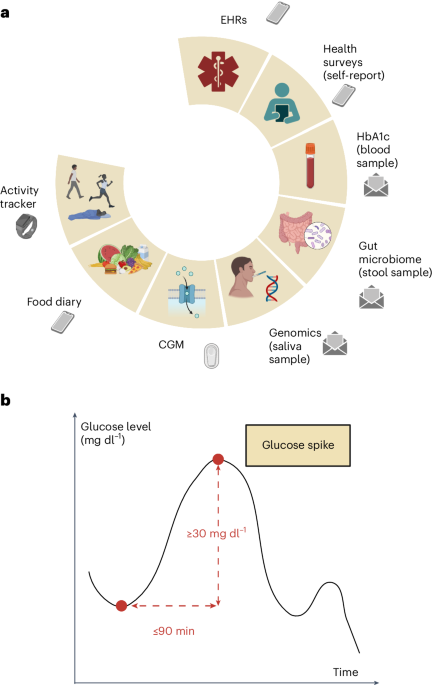
What made this study different is that everything happened remotely. For ten days, participants wore a continuous glucose monitor (CGM) and a fitness tracker at home, collecting data on glucose levels, sleep, heart rate, and physical activity. They also used mobile apps to log meals and share their electronic health records, and they sent in self-collected saliva, blood, and stool samples for testing (Figure a).
This approach allowed us to create a diverse, fully remote cohort, with nearly half the participants coming from groups typically underrepresented in biomedical research.
What we found
In this study, we set out to explore how different factors (such as age, activity level, and gut health) relate to changes in blood sugar levels, and to integrate multimodal data to build a more complete picture of individual risk for T2D.
We looked closely at glucose spikes - rises in blood sugar that typically occur after meals (Figure b) - as well as other glycemic measures. These metrics showed clear differences depending on whether a person was healthy, had prediabetes, or had T2D. Interestingly, people with prediabetes tended to have glucose patterns more similar to healthy individuals than to those with T2D. But even within each group, we saw a wide range of responses, highlighting how varied and complex blood sugar regulation can be.
We also observed that people with greater gut microbiome diversity and higher levels of physical activity generally had healthier blood sugar responses. On the other hand, a higher body mass index, older age, and higher resting heart rate were linked to less favorable glucose patterns.
By combining all this information using an AI model, we discovered that two people with the same HbA1c can still have very different risk profiles. Our AI model helped build individualized glycemic risk profiles that better reflect a person’s true metabolic state than traditional lab tests alone.
Overall, our findings highlight how many different factors affect blood sugar control and support the need for more personalized strategies to prevent and manage T2D.
Why it matters
We demonstrated that collecting diverse health data remotely is not only feasible but also deeply informative. As wearable sensors, mobile apps, and at-home testing become more widespread, we now have the tools to monitor health continuously, moving beyond the snapshot provided by occasional clinic visits.
This study marks an important first step toward more inclusive and scalable ways to prevent and monitor T2D, especially now that CGMs and other wearables are gaining traction among the broader population, not just those already diagnosed.
Looking ahead
The PROGRESS study uncovered meaningful associations between glucose spikes and multiple demographic, metabolic and lifestyle factors. The next step is to investigate the underlying causal relationships among these variables and to validate our approach in longitudinal and prospective studies.
Our findings, combined with advancements from future research, could offer valuable insights for tailoring interventions, supporting preventive lifestyle programs, and improving risk stratification. Together, these efforts could play a crucial role in reducing the prevalence of T2D and prediabetes.
Follow the Topic
-
Nature Medicine

This journal encompasses original research ranging from new concepts in human biology and disease pathogenesis to new therapeutic modalities and drug development, to all phases of clinical work, as well as innovative technologies aimed at improving human health.
Related Collections
With Collections, you can get published faster and increase your visibility.
Stem cell-derived therapies
Publishing Model: Hybrid
Deadline: Mar 26, 2026
Digital Medicine for Infectious Diseases
Publishing Model: Hybrid
Deadline: Nov 09, 2026
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in