Perspective: A Cancer Immunologist in a Molecular Imaging Lab
Published in Cancer
When I started graduate school, I had several preconceived notions about how tumors respond to immune checkpoint blockade (ICB). Tumors that are sensitive to ICB are known as “hot” tumors, while tumors that did not respond to ICB are considered “cold” tumors. When I accepted this project, my goal was to uncover a way to identity such “cold” tumors, and, if things went well, a way to mitigate their resistance to ICB. Instead, it seems like my work simply raised more questions than it answered.
I started with two tumor models: B16-F10 and 4T1. B16-F10 is a murine melanoma tumor model known to be somewhat sensitive to combination programmed death-1 (anti-PD-1) and cytotoxic T-lymphocyte associated protein-4 (anti-CTLA-4) blockade, whereas 4T1 is a murine breast cancer model known to be resistant to the same treatment combination. For 4T1 to be resistant to anti-PD-1 and anti-CTLA-4, two immunotherapies that rely on T cell function which in turn are inhibited by acidic tumor microenvironments, it follows that 4T1 tumors are more acidic than B16-F10 tumors. Right off the bat I was mistaken. Initial screening Seahorse data showed that the average baseline proton efflux rate of B16-F10 cells is approximately twice that of 4T1 cells.
This is also a good time to take a step back and reflect on what makes a good scientist and what makes a good mentor. At this time in my life, I worked under the tutelage of five principal investigators of different fields and varying student successes. And unfortunately, there was a time when I presented data that showed a treatment combination was unsuccessful and was told that I either have poor technique or that I ought to try a different model of the same cancer type. Thankfully that project did not move forward. But Dr. Mark Pagel saw things differently. Instead of finding a model to fit my narrative, he encouraged me to see things through and see what is born of the data. And that is something worth passing down to the next generation of scientists: that our goals and value is not defined by publications, but by our tenacity and wisdom to find the story the science is trying to tell us.
And the science was adamant on telling a story that subverted my expectations. Esomeprazole should reduce the proton efflux rate of both B16-F10 and 4T1 cells. No. Treating tumors will esomeprazole simultaneously with anti-PD-1 and anti-CTLA-4 should have the greatest antitumor effect as doing so will maximize the time of effect for all treatments. Try again. Highly acidic tumors are the most active as a result of the Warburg effect and would therefore result in the largest, most resistant tumors. But not really. After some time, it was as if the only consistency was inconsistency.
I think part of Dr. Pagel’s resiliency as a scientist is the simple fact that he is a trained chemical physicist. In fact, he taught a class on quantum mechanics. Now in my time training under him I asked him many, many questions about how MRIs work. But I will never ask him about quantum physics. One of my first lessons was that protons spin, but that protons don’t really spin, except the spin nature of protons is what drives MRI, and now the fear is in me. Something about the duality of nature probably imbues him with a broad perspective and a wry sense of humor. Am I saying that all cancer immunologists should work with a molecular imaging specialist? It is refreshing, in a painful sort of way.
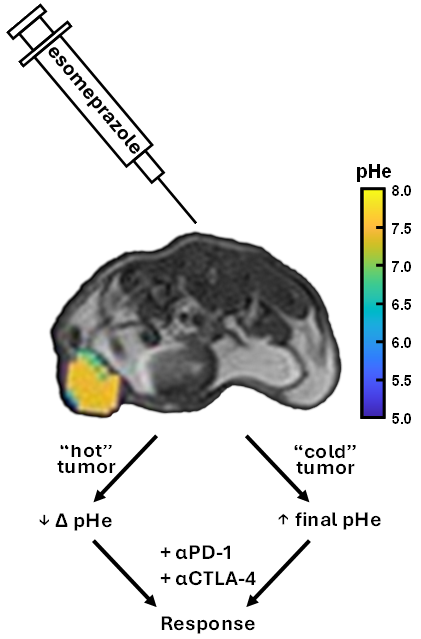
Despite the contradictory nature of my work, the story really became clear when I took a step back and digested the data. B16-F10 and 4T1 tumors were bound to respond differently simply due to the contrast in their tumor biologies. B16-F10 cells likely did not respond as robustly as 4T1 cells did to esomeprazole since B16-F10 cells do not engage vacuolar ATPase to acidify the tumor and contribute to ICB resistance. Furthermore, B16-F10 tumors likely did not respond to esomeprazole by reducing its frequencies of Ly6C+ monocytic myeloid-derived suppressor cells as the frequencies of those cell populations are already almost one-third that of the 4T1 tumors at baseline. This may go on to also explain why B16-F10 tumor response correlates to the change in pH rather than the final pH as 4T1 tumors do. Seahorse data established that 4T1 cells are highly susceptible to esomeprazole acidification control, while B16-F10 cells are not. Because 4T1 cells are more sensitive to esomeprazole, the tumor pHe prior to esomeprazole matters less since the cancer cells will respond in a TCF-1+ T cell-mediated manner. On the other hand, the change in pHe for B16-F10 tumors correlates to tumor control because how the tumors responded to esomeprazole matters. The greater the response, the more tumor control and the smaller the B16-F10 tumor. B16-F10 tumors were inherently different from 4T1 tumors, and those differences must be heavily considered when reviewing the data.
B16-F10 was my “hot” tumor model and 4T1 was my “cold” tumor model in this project. But there are nuances to these categories that need to be revealed to move forward unlocking ICB. As mentioned previously, some B16-F10 tumors responded to esomeprazole when the Seahorse data showed no significant difference in proton efflux rate following esomeprazole treatment. Whether that is a result of heterogeneity in the cell population, or a tumor adaptation is unclear. This does, however, highlight different degrees of “hot”-ness that needs further evaluation. But to improve this strategy of patient stratification by tumor susceptibility to esomeprazole and ICB, it is unclear whether to classify tumors as 4T1-like (tumor response correlates to final pHe) or B16-F10-like (tumor response correlates to change in pHe). Should a tumor biopsy be taken before and after esomeprazole to ascertain Ly6C+ monocytic myeloid-derived suppressor cell and CD8+ T cell frequencies in addition to acidoCEST MRI? Should all tumor biopsies undergo Seahorse screening? That is a question for the next graduate student.
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in