Point-of-Care Artificial Intelligence-enabled ECG for Dyskalemia: A Retrospective Cohort Analysis for Accuracy and Outcome Prediction
Published in Healthcare & Nursing
Potassium (K+) is the main cation maintaining the electrical gradient across cell membranes. The membrane potential created by K+ allows cells to generate action potentials, which is critical for heart function. The concentration of K+ in plasma is carefully regulated between the intracellular and extracellular fluid and by renal K+ excretion. Low potassium (hypokalemia) and high potassium (hyperkalemia) are commonly seen in the emergency department,1 the extremes of which can cause life-threatening arrhythmias. However, traditional laboratory tests take more than half an hour to obtain results and many patients have suffered sudden cardiac death while awaiting their blood potassium test.2

The current treatment guideline for hyperkalemia prioritizes electrocardiography (ECG) to look for dangerous changes and initiate rapid treatment to save life.3 However, morphologic ECG changes associated with dyskalemias (high or low potassium) may not be easily recognized even by experienced physicians or cardiologists. Using deep learning models (DLM), which have revolutionized artificial intelligence (AI) elsewhere, we have developed a system called ECG12Net for the rapid quantitative estimation of blood K+ concentration in the ED,4 which provides a prediction within 1 minute.
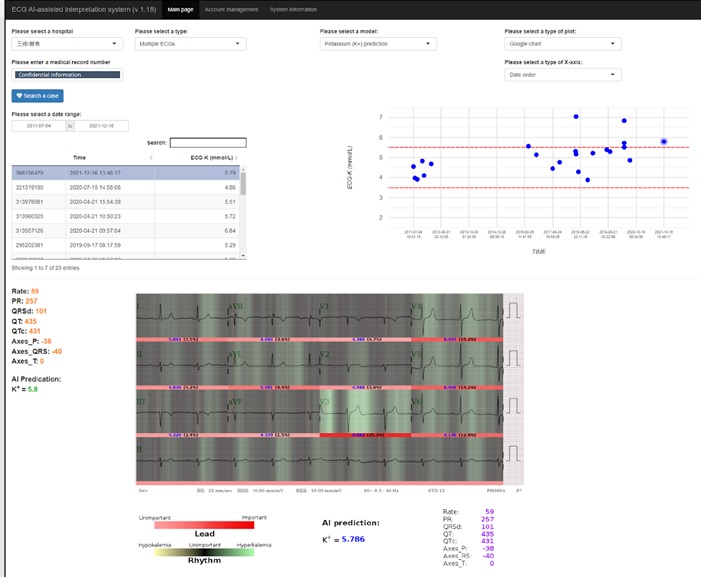
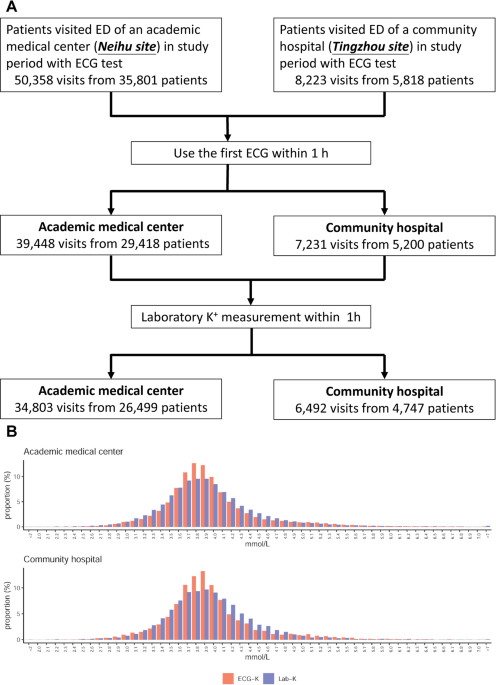
On January 19th, 2022, we published the paper “Point-of-Care Artificial Intelligence-enabled ECG for Dyskalemia: A Retrospective Cohort Analysis for Accuracy and Outcome Prediction” in npj Digital Medicine. The foundation for this project was our AI-enabled ECG system for predicting serum potassium (Figure 1), which provided decision support for first line clinicians. Our clinicians could use this system to obtain a ECG-K+ within 1 minute and monitor patients over time. The system also highlighted suspicious areas of the ECG when physicians selected an ECG (Figure 2). We then analyzed the clinical impact of this tool on real patients, which showed that the system is quite accurate. As shown in the Figure 3, our AI-enabled ECG system rapidly calculated ECG-K+ for point-of-care support in the ED and achieved comparable accuracy to previous studies4,5 in detecting moderate to severe dyskalemia.
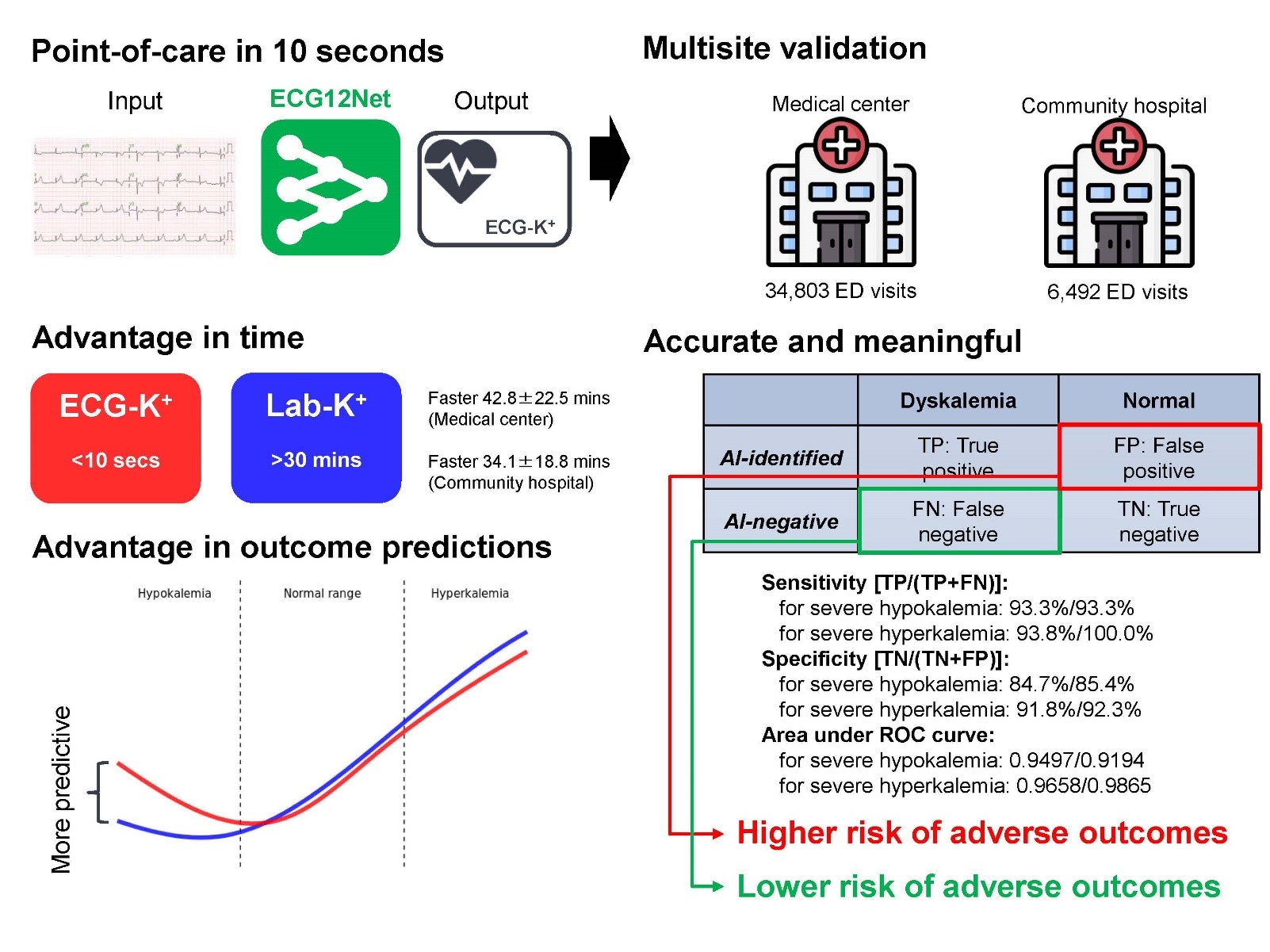
One major criticism of AI systems is the handling of false positive predictions, which may cause anxiety, inconvenience, and even possibly inappropriate management of the patients.5 With this in mind, we feel the most meaningful contribution of this study is not just documenting the accuracy of our ECG-K+ system, but rather, the new perspective we bring to discordance between ECG-K+ and Lab-K+. We found that when ECG-K+ and Lab-K+ were discordant, ECG-K+ was more predictive of subsequent all-cause mortality, hospitalizations, and ED revisits. This multi-site retrospective study not only validated the accuracy of ECG-K+, especially in moderate to severe dyskalemia, but also revealed meaningful differences between ECG-K+ and Lab-K+.
Taken together, our data show that ECG-K+ may be useful as a background system actively monitoring every ECG. The approximately half hour lead time afforded by ECG-K+ means severe dyskalemias can be prioritized in physicians’ minds, potentially life-saving interventions readied at the bedside, and given immediately upon receipt of a concordant lab result. If the results are discordant, these are still opportunities for physicians to think more carefully about the patients’ underlying conditions due to the higher mortality and other adverse outcomes.
For more about our work, please find the complete study in npj Digital Medicine: https://www.nature.com/articles/s41746-021-00550-0
References
1 Conway, R., Creagh, D., Byrne, D. G., O'Riordan, D. & Silke, B. Serum potassium levels as an outcome determinant in acute medical admissions. Clinical medicine (London, England) 15, 239-243, doi:10.7861/clinmedicine.15-3-239 (2015).
2 Kovesdy, C. P. et al. Serum potassium and adverse outcomes across the range of kidney function: a CKD Prognosis Consortium meta-analysis. European heart journal 39, 1535-1542, doi:10.1093/eurheartj/ehy100 (2018).
3 Lott, C. et al. European Resuscitation Council Guidelines 2021: Cardiac arrest in special circumstances. Resuscitation 161, 152-219, doi:10.1016/j.resuscitation.2021.02.011 (2021).
4 Lin, C. S. et al. A deep-learning algorithm (ECG12Net) for detecting hypokalemia and hyperkalemia by electrocardiography: algorithm development. JMIR medical informatics 8, e15931, doi:10.2196/15931 (2020).
5 Galloway, C. D. et al. Development and validation of a deep-learning model to screen for hyperkalemia from the electrocardiogram. JAMA cardiology 4, 428-436, doi:10.1001/jamacardio.2019.0640 (2019).
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in