Polycystic Ovary Syndrome Among Indian Women
Published in General & Internal Medicine and Public Health
Explore the Research
Just a moment...
www.thelancet.com needs to review the security of your connection before proceeding.
A "functional cyst" is an ovarian cyst formed when the ovary does not release the ovum and instead forms cysts filled with fluid and ovum. The presence of multiple cysts in the ovary is termed as PCOS which obstruct the menstrual cycle called amenorrhea, hamper conception and pregnancy loss. Based on the observed population and criteria, 8–13% of people worldwide have PCOS. The frequency of PCOS varies throughout India between 3.7% and 22.5% depending on the demographics and conditions. Uncertainties in diagnosis arise because some women have PCOS without cysts. Due to lack of awareness, a large number of teenage and young women in India do not visit gynecologists for routine checkups and remain undiagnosed. Late diagnosis of PCOS comes up with other problem like infertility, sleep apnea, depression, obesity, metabolic syndrome, cardiovascular problems, endometrial cancer, fatty liver and hepatitis and its associated complications.
PCOS is a systemic condition with poorly understood etio-pathologies, aside from reproductive pathology. Insulin resistance is more common in women with PCOS, and it's unfortunate that there is little information available about the mechanism underlying PCOS-induced diabetes and etiology-specific treatments. The faulty gene that causes the impaired metabolic pathway is the cause of PCOS and ovarian dysfunction. Restoring ovulation and treating hirsutism with hormonal contraceptives and antiandrogens are the main treatment modalities for PCOS.
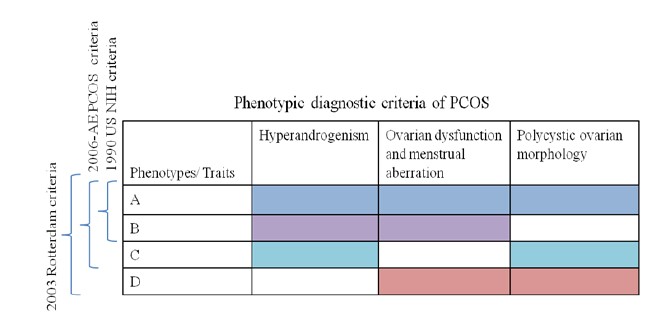
Three organizations have defined the diagnostic criteria for PCOS: the Androgen Excess and PCOS Society (AE &PCOS), the European Society for Human Reproduction and Embryology/American Society for Reproductive Medicine (ESHRE/ASRM), also known as the "Rotterdam Criteria," and the National Institutes of Health/National Institute of Child Health and Human Disease (NIH/NICHD). The AE & PCOS defined clinical and/or biochemical hyperandrogenism (HA) and ovarian dysfunction as menstrual aberration [anovulatory oligomenorrhea (AnO) and or existence of polycystic ovary morphology (PCOM)] correlated with transvaginal ultrasound (TSUS). These parameters classify PCOS phenotypes into three categories: A, B, and C. A covers (HA, AnO, and PCOM), B and C only include two (HA and AnO or HA and PCOM, respectively), while AnO and PCOM were included in the fourth criteria D
The diagnosis of PCOS is difficult due to differences in endocrine and clinical measurement as well as a lack of clear collective criteria. Women with PCOS often have HA, which is a common symptom of androgen receptor dysfunction and impaired androgen signaling. Serum levels of luteinizing hormone (LH), follicle stimulating hormone (FSH), and the number of cysts in an ovarian morphology with polycystic ovarian pattern are all correlated with androgen signaling. The aberrant androgen receptor also exhibits subfertility, an extended oestrous cycle, and increased pre-antral and atretic follicles. The primary cause of PCOS is an elevated level of gonadotropin-releasing hormone (GnRH) and a high LH to FSH ratio. Furthermore, a number of additional factors, including environmental factors, epigenetics, and insulin resistance (IR), support the notion that metabolic disorders, cardiovascular risk, diabetes and depression. PCOS etiopathologies are influenced by genetic, endocrine, and environmental factors. Given that PCOS is a heterogenetic and multifactorial disorder, different patients within a family have differing genetic susceptibilities to particular genes. For complex PCOS, genetic screening for particular biomarker genes and linkage analysis are not feasible.
In order to improve the quality of care, a nation must establish biological reference intervals for hormonal parameters. Failing to do so may lead to unnecessary spending or the denial of care to those who require it. It is challenging to determine the normative range of different hormones in reproductive-aged Indian women due to the country's high population heterogeneity. According to a Pan-India study that was published in The Lancet Regional Health - Southeast Asia 2023, the majority of analyzed participants (after excluding hormonal imbalance and comorbities) were unemployed (64.8%) and belonged to the lower and middle socioeconomic classes (31%). Different population of women who are of reproductive age have slightly different normative ranges for PCOS relevant hormones[i]. Hopefully, this study will bridge the gap in normative hormonal data among reproductive-age Indian women and pave the way for the development of the best possible diagnosis and treatment plan.
[i] Ganie, M. A., Chowdhury, S., Suri, V., Joshi, B., Bhattacharya, P. K., Agrawal, S., ... & Suresh, A. (2023). Normative range of various serum hormonal parameters among Indian women of reproductive age: ICMR-PCOS task force study outcome. The Lancet Regional Health-Southeast Asia, 15.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in