Rethinking Trust, Privacy, and Power in Digital Health Collaborations
Published in General & Internal Medicine, Statistics, and Business & Management

Public-private partnerships (PPPs) are often hailed as engines of innovation in digital health. By combining the expertise of academic hospitals and other public institutions with the resources of technology companies, they promise solutions for some of healthcare’s biggest challenges. But these collaborations come with their own set of complex ethical questions—questions we felt are not yet adequately addressed by existing guidelines despite recent academic publications on the topic.
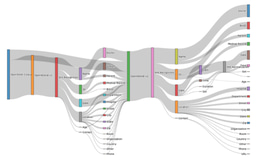
In our paper, published in npj Digital Medicine, we conducted a scoping review of 46 studies exploring the ethical dimensions of digital health PPPs. Our goal was to systematically map the landscape of concerns, identify recurring themes, and offer recommendations for more ethically informed and publicly trusted partnerships.
What we found
We were struck by how much the ethics discourse is shaped by headline-grabbing cases—like the NHS and DeepMind partnership or Iceland’s collaboration with deCODE Genetics. These examples vividly illustrate how partnerships can falter when ethical concerns are overlooked: failures in transparency, unclear data governance, or insufficient consent mechanisms not only threaten individual privacy but erode public trust in both public and private institutions. However, these cases focus on the responsibility of companies, and especially on ‘worst practices’; while our review also highlighted best practices in PPPs as well as the role of governments, who sometimes also have (economic) interests that can conflict with those of citizens and patients who participate in digital health research and whose data is used.
From our analysis, three core themes emerged:
- Privacy and Consent – Sharing health data between public and private organizations, even in de-identified form, raises ethical issues. Many participants are not comfortable with commercial use of their data. The literature shows that improvements to informed consent processes are needed to mitigate privacy concerns of data subjects.
- Public Benefit and Access – Many partnerships appeal to “the public interest” to justify data use—but what does that really mean? Our study reveals that limited consensus exists on what constitutes public “interest” or “benefit” or how it should be distributed. In some cases, economic goals such as boosting national competitiveness could overshadow direct health improvements.
- Governance and Trustworthiness – Governance frameworks for digital health PPPs are underdeveloped. Ethics boards often lack domain-specific expertise, and the role of the public sector as data steward is not well defined. Our review highlights the need for greater transparency, stakeholder engagement, and clearer oversight mechanisms.
Why this matters
PPPs will continue to play a central role in digital health innovation. But without a clear ethical framework, these partnerships risk repeating the mistakes of the past—or worse, losing public trust entirely. In the paper we propose 15 practical recommendations, ranging from requiring opt-in consent for commercial data use to ensuring public ownership of health data assets.
One of our most important insights is that ethical responsibility doesn’t just lie with the private sector. Public institutions must also be held accountable for how they define and pursue the public interest. In fact, we argue that it’s time to broaden the conversation from concerns about “Googlization” of health to a deeper interrogation of the economization of public health itself.
Behind the scenes
This paper was born out of a shared sense of urgency between researchers at the Institute for History and Ethics in Medicine, TU Munich, Germany, one of whom also works at Amsterdam UMC, the Netherlands. Working as ethicists in research consortia with commercial partners, we have first-hand experience of both benefits and downsides of PPPs, and we wanted to review these aspects independently of a specific consortium. We found there was no space yet where these concerns were systematically addressed, so we conducted this literature review. The systematic search was led by Daan Horbach for his master’s thesis in Philosophy, Bioethics and Health (VU University, Amsterdam). He explains his interest in the topic and what he learned:
“While I had no prior relevant research where I encountered issues about PPPs, I already had an interest in the ethics of digitalization in healthcare. Furthermore, at the time I worked for a medical clinic where partnerships with different private parties were the norm. Often within these partnerships and contracts, topics such as privacy or the empowerment of patients/employees were used to show the ‘benefit’ of using their product. When I had the possibility to partake in this study, I knew that it was an opportunity that I could not pass. Working on this article has been a great start to open up the world of academia to me.”
Looking ahead
We hope our findings will inform both researchers and policymakers involved in digital health PPPs. We see this work as a starting point—not a final word. In future projects, we plan to explore more inclusive partnership models, such as tripartite partnerships where patient groups and civil society organizations are formally involved as equal partners. We also call for the development of international ethics guidelines tailored to the specific complexities of digital health. Furthermore, we are applying for research grant to conduct ‘embedded ethics’ research in specific partnerships to further explore topics like public benefit.
At a time when trust in both public and private institutions can be fragile, we believe transparency and community engagement aren’t optional—they’re essential to the long-term success of digital health partnerships.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in