SDG 3: Sickle Cell Disease and its Impact on the Black community
Published in Sustainability and General & Internal Medicine
Poster image: © Ezume Images / stock.adobe.com
What is Sickle cell disease, and how does it disproportionately affect the Black community?
Sickle cell disease affects the Black community in a way that is unparalleled. It has been argued that the disease has been underfunded in research for years, leading to more cases worldwide.
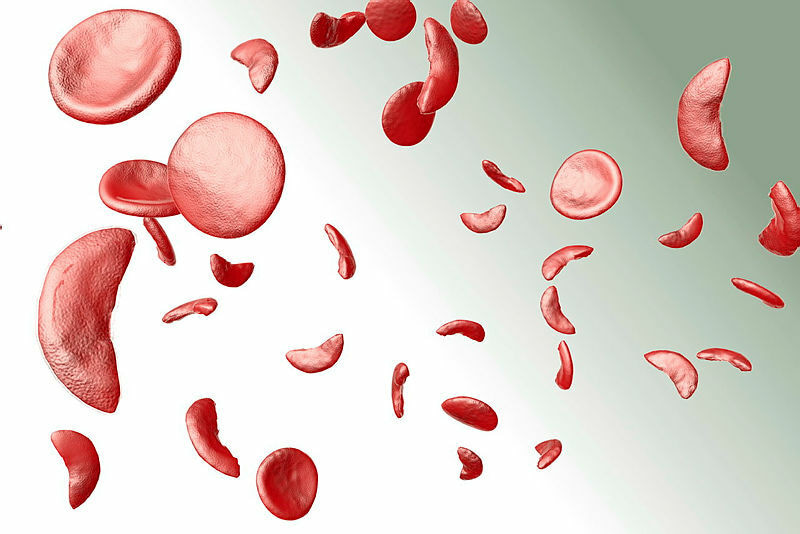
Sickle cell anemia is a genetic blood disorder caused by a mutation in a gene that leads to the production of abnormal hemoglobin. This makes red blood cells sticky and misshapen, resembling a sickle, and they are destroyed faster than they can be replaced. This can block blood flow, causing severe pain, a higher risk of infections, and potential organ damage.
Sickle cell disease disproportionately affects the Black community due to genetic factors. In regions where malaria is or was common, having the sickle cell trait offers a survival advantage, as people with the mutated gene are less likely to develop severe malaria infections.
How can we raise awareness about Sickle cell disease within the Black community and beyond?
GP surgeries play a crucial role in raising awareness and highlighting the impact of Sickle cell disease on individuals. Traditionally, awareness is spread through posters in health establishments, but it’s also important to use social media, schools, and local shops in areas with large Black communities. Ground-breaking television series' like Supacell (2024) have sparked important conversations within the community, leading more people to seek information. However, more can still be done. The National Health Service (NHS) and other services should collaborate with local patient advocacy and research groups to provide additional information and support.
What can individuals, organisations, and the broader community do to support people living with Sickle cell disease?
A greater understanding of the symptoms of illnesses affecting Afro-Caribbean communities, such as prostate cancer, diabetes, and fibroids, has helped bring more awareness to these issues. While these conditions are not exclusive to these communities, raising awareness has been important. Additionally, support services can offer financial assistance and transportation for hospital visits.
How does the lack of awareness and education about Sickle cell disease affect early diagnosis and treatment?
The lack of recognition and understanding of the illness by various parties often leads to misdiagnosis. This lack of awareness and education means people are unaware of their own biological makeup. In Nigeria, it is common practice to get tested to know your genotype and whether you're a carrier. People often ask about it when dating and getting serious! Being aware helps foster open conversations during family planning, allowing people to understand how they can support and care for their children.
The lack of awareness also affects early diagnosis, as many people do not recognise the symptoms. If informative conversations were held to highlight the early symptoms, treatment and diagnosis could happen much sooner.
What are the specific barriers Black communities face in accessing life-saving treatments for Sickle cell disease, and how can these barriers be overcome to reduce premature mortality?
There has always been a certain level of distrust towards the medical profession, not just in the UK, but globally. This has led to caution and the need to consult external sources before seeking help, often insisting on second opinions when receiving medical advice.
Unfortunately, racism in healthcare remains a significant issue. There have been troubling reports of recurring instances of racial profiling, resulting in incorrect diagnoses and inadequate care. One way to address this is by establishing benchmarks set by patient advocacy groups that medical teams must adhere to.
How can we ensure that people living with Sickle cell disease receive holistic care that includes not only physical treatment but also the mental health support needed to improve overall well-being?
GPs need to be better equipped to connect people with the resources they need, with more community outreach and clearer information on available services in local areas.
Costs are a factor, so it's important to communicate clearly that this care is essential, with stronger and more effective communication from healthcare providers.
There also needs to be greater awareness among all clinicians who interact with sickle cell patients, especially during a crisis. The initial assumption that the patient is addicted to opiates must be challenged and corrected.
How can we build a stronger sense of solidarity and advocacy for Sickle cell disease in the Black community?
There should be more contributions and stronger connections between healthcare services and charities focused on Sickle cell. Areas with a significant Afro-Caribbean population, like Lambeth, often host events that help raise awareness of these organisations.
We need to talk more openly, as there's often a tendency to remain silent or secretive, especially about illness. Conversations can take place in places like barbershops, hairdressers, and schools. It's important to reach out to family and friends and create safe spaces where people can discuss and interact with those affected by Sickle cell, showing that we care about what they're going through. Talk, share, and use social media to spread awareness.
Additionally, having specialist haemoglobinopathy practitioners who work with, educate, and advocate for patients is crucial.
In terms of SDG 3.4, how can the medical research community accelerate efforts to find a cure or more effective treatments for Sickle cell disease, thus reducing premature mortality rates?
There should be more targeted funding for research in this area, with support for studies in Africa, the Caribbean, and diaspora communities.
Closer collaboration with charities is essential, but it’s also important to engage with diplomatic entities and focus on regions and boroughs with high populations that are most affected by the disease.
In May 2024, the drug Voxelotor was approved by the NHS for eligible patients. Taken once a day, it can reduce the need for blood transfusions and lead to fewer hospital visits. Additionally, in January 2025, a ground-breaking gene-editing treatment was approved by the NHS. Studies suggest that this one-off gene therapy offers the potential for a cure. These innovative treatments must be rolled out globally by policymakers and the medical research community.
What are the key steps we can take to integrate Sickle cell disease care into national health policies in a way that reduces its impact on premature mortality?
Raising awareness of Sickle cell within the NHS has traditionally been done through various media outlets. Since the disease primarily affects a "minority" group, targeted videos, posters, and radio ads in healthcare settings seem to be an effective approach.
The pharmaceutical industry and institutions training current and future clinicians must encourage research on sickle cell as part of their academic work. This will help ensure that practitioners are supported in delivering evidence-based clinical care.
Interview created, formatted and edited by India Sapsed-Foster, Associate Publisher and a network organiser of Springer Nature's Black Employee Network (SN BEN)
Responses from members of SN BEN: Abiola Lawal (Senior Publisher) Flora Okumagba (Project Manager, Engineering), Marlene Stewart (Director, Content Partnerships, Scientific American) and Clive Wilson (Infrastructure Monitoring Analyst, Workplace Enablement)




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in