
Explore the Research

Sniffing oxytocin: Nose to brain or nose to blood? - Molecular Psychiatry
Molecular Psychiatry - Sniffing oxytocin: Nose to brain or nose to blood?
Oxytocin (OXT) is a hypothalamic neuropeptide/hormone most well-known for its role in childbirth following release into the blood from the pituitary. However, over the last few decades, the effects of OXT on the brain and social behavior have been at the forefront of interest in human neuropsychopharmacology and social neuroscience research with many studies reporting that it has an important modulatory influence on social motivation and cognition, including enhancing trust, social co-operation and learning, emotion recognition, empathy, increasing the pleasure of social touch and perceived attractiveness of partners and even helping to reduce conflict between them. OXT has thus often been labelled as a “love hormone”, “cuddle hormone”, or “trust hormone”. From a translational point of view, a number of disorders with social problems appear to have reduced OXT signaling and administering OXT intranasally as a potential treatment has been reported to produce improvements in some clinical trials involving individuals with autism, Prader-Willi syndrome and schizophrenia.
An intranasal route of OXT administration has been adopted by the majority of studies in humans since evidence suggests that in this way it can penetrate directly into the brain by circumventing the blood–brain barrier (BBB). However, it is still unclear how functional effects are mediated since intranasal OXT can both directly enter the brain directly (nose to brain) via the olfactory and trigeminal nerves and increase peripheral vascular concentrations (nose to blood) via absorption into nasal and oral blood vessels. Whereas it was previously thought that OXT in the peripheral circulation could not easily cross the BBB, new research has shown that it can do so by binding to the receptor for advanced glycation end products (RAGE). Additionally, many peripheral organs and nerves have OXT receptors, most notably in cardiovascular and gastrointestinal systems which can influence the brain via the vagus nerve, and so increased peripheral OXT concentrations could influence the brain indirectly in this way too. Indeed, some studies in both animal models and humans have reported that OXT administered via peripheral routes which do not permit direct entry into the brain (i.e. intravenous, subcutaneous or oral) can produce similar functional effects as seen after intranasal administration. Thus the observed functional effects of intranasal OXT may be contributed to by either the “nose to brain” route or the “nose to blood” route or both. The relative functional contributions of these routes are not established and have received insufficient attention in the field.
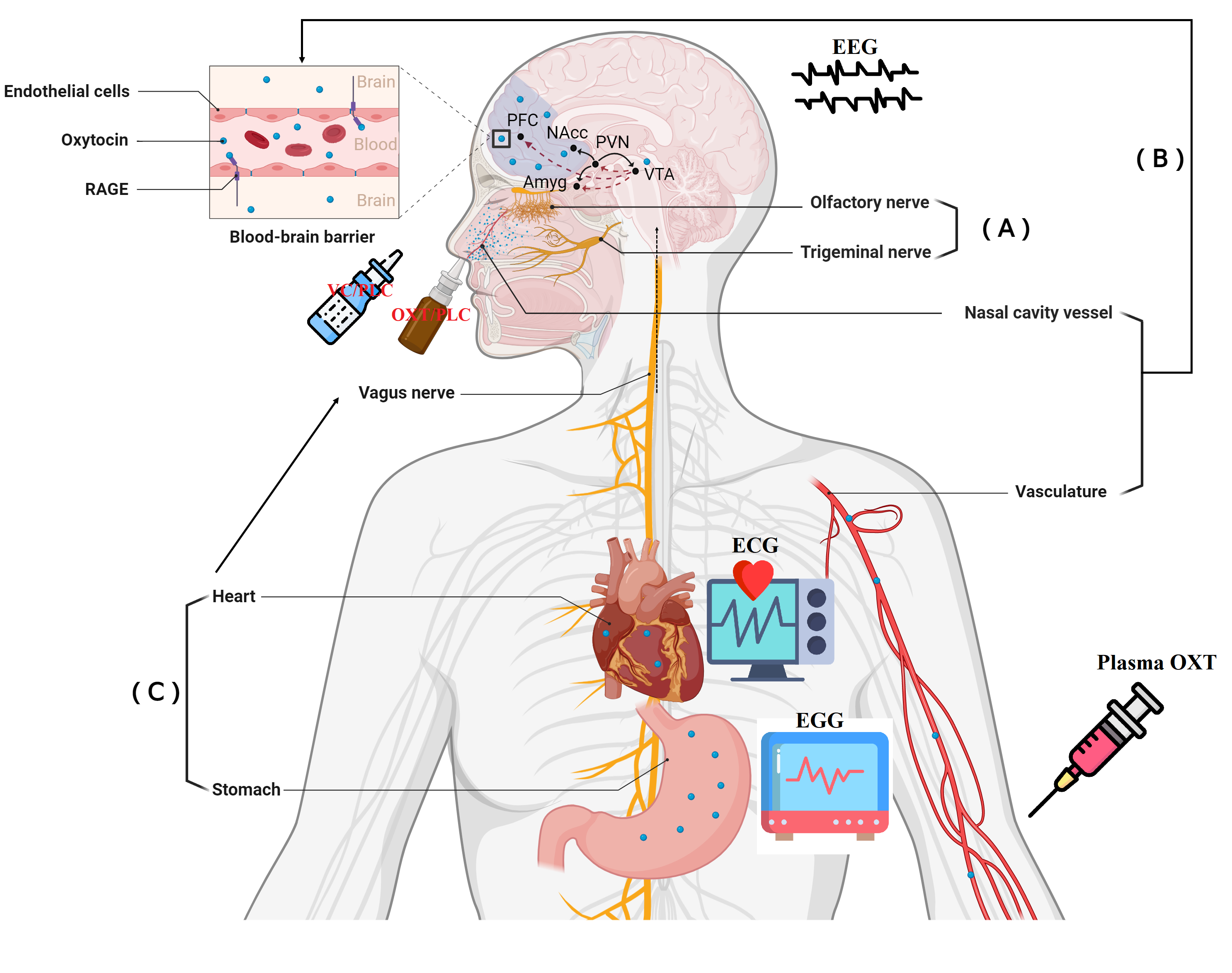
Illustration of routes of intranasally administered OXT producing its functional effects and neural and peripheral measures in the present study
Given methodological limitations in human studies, one possible approach to disentangle the above question is to restrict intranasal OXT to only produce its potential functional effects via direct entry into the brain by preventing it from entering the peripheral circulation. To achieve this, we used a novel approach of pretreatment with a vasoconstrictor (VC) to reduce the ability of intranasal OXT to increase peripheral concentrations but without influencing penetration directly into the brain. We first confirmed the effectiveness of this strategy by showing that pretreatment with the VC markedly reduced the normal increase in blood concentrations of OXT following a single 24 IU intranasal dose. We next investigated whether observed effects of intranasal OXT on brain cortical electrical activity were affected by using the VC to reduce the amount of intranasal OXT entering the blood using electroencephalography (EEG). We found that intranasally administered OXT compared to placebo treatment produced extensive increases in cross frequency coupling (CFC) between low (delta) and high (beta) frequency EEG component from 15-60 min post treatment. Delta-beta CFC is proposed to reflect subcortical-cortical crosstalk, particularly the interplay between emotional/motivational systems and cognition, which corresponds well to the demonstrated role of OXT in modulating social motivation and emotion. Pre-treatment with the VC on the other hand prevented intranasal OXT from producing these extensive overall effects on increasing delta-beta CFC. Furthermore, the observed effects of intranasal OXT on delta-beta coupling occurred over the same time course as the increases in blood OXT concentrations and magnitude of changes in delta-beta CFC were associated with the magnitude of increased OXT concentrations in the blood. Taken together these findings suggest that it is the nose to blood rather than the nose to brain route which is important for intranasal OXT to influence brain function.
So how might increased peripheral concentrations of OXT be producing these functional effects on delta-beta CFC? While we could not directly address this question in the current study, we did additionally record whether intranasal treatment influenced resting state autonomic nervous system activity which might indicate whether it was acting on peripheral receptors in the heart and gastrointestinal system to promote vagally-mediated stimulation of the brain. To this end, we also measured changes in heart rate variability, skin conductance response and electrogastrogram as peripheral vagal/parasympathetic markers but did not find any significant effects of OXT either alone or with the VC pre-treatment compared to the placebo treatment. Thus, at this stage our findings suggest that the neural effects of intranasal OXT following its induced increased concentrations in the blood may be due to it binding to RAGE and crossing the BBB to enter into the brain and act on its receptors there, although this would need to be confirmed by further experiments.
Overall therefore, our findings suggest a critical role of peripheral vasculature-mediated routes in the functional actions of intranasal OXT, possibly as a result of OXT crossing the BBB into the brain. From a translational point of view, since our findings indicate that intranasal OXT may produce functional effects following increased peripheral concentrations rather than after direct entry into the brain this opens up consideration of whether other routes of administration such as oral or intravenous which can only increase peripheral vascular concentrations might be used as potential interventions in psychiatric disorders with social dysfunction.
Follow the Topic
-
Molecular Psychiatry

This journal publishes work aimed at elucidating biological mechanisms underlying psychiatric disorders and their treatment, with emphasis on studies at the interface of pre-clinical and clinical research.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in