The association of body composition and fat distribution with dysmobility syndrome in community-dwelling older adults
Published in Healthcare & Nursing, Biomedical Research, and Public Health
Dysmobility Syndrome (DS) is a condition characterized by the accumulation of clinical risk factors for functional disability, including osteoporosis, sarcopenia, and obesity. Additionally, neurological disorders affecting the motor and sensory systems can contribute to DS, leading to gait disturbances, muscle weakness, and an increased risk of falls and fractures. Despite the known impact of body composition on DS, the role of fat distribution in different body regions remains unclear.
This study aimed to investigate the association between regional fat mass distribution and the likelihood of DS in older adults. Conducted as part of the second phase of the Bushehr Elderly Health (BEH) Cohort, this cross-sectional study defined DS based on the presence of at least three criteria associated with the syndrome. Body composition was assessed using dual-energy X-ray absorptiometry (DXA) and anthropometric measurements, while multivariate logistic regression and adjusted univariate linear regression analyses were applied to explore these relationships.
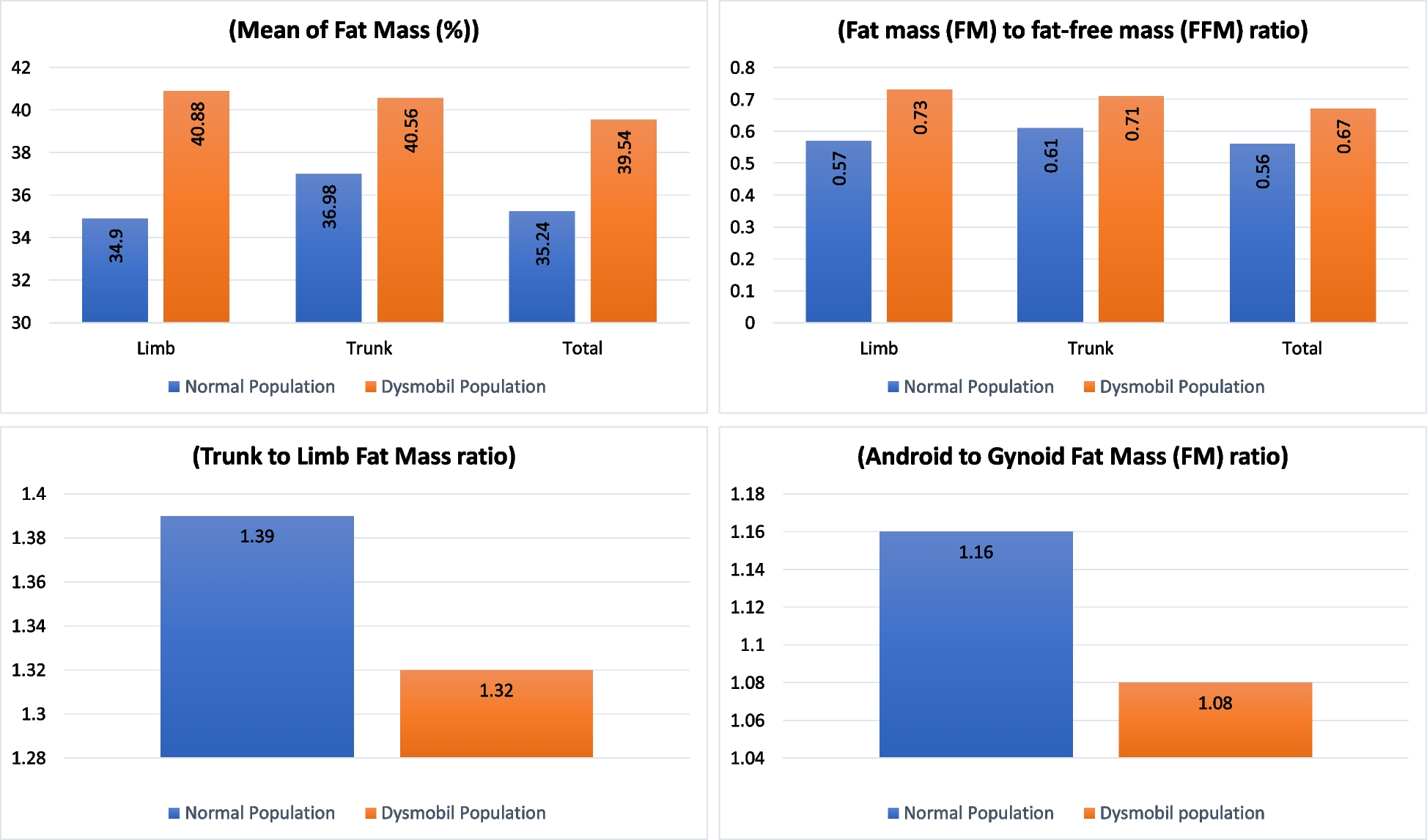
Among 2,359 participants, 1,277 individuals (54.13%) were diagnosed with DS. The final logistic regression model revealed a significant association between DS and both fat mass (FM) and the FM-to-fat-free mass (FFM) ratio in the limbs region, with stronger associations observed in this region compared to the trunk. Specifically, higher fat mass in the limbs, particularly in the legs, was associated with increased odds of DS. Conversely, a higher android-to-gynoid fat mass ratio was linked to a lower risk of DS.
These findings highlight the critical role of regional fat distribution in DS risk among older adults. Our results suggest that monitoring fat mass, particularly in the limbs, may serve as an effective strategy for early DS detection and intervention. By implementing targeted screening and preventive measures, healthcare professionals can reduce disability risks and improve the quality of life in aging populations.
Follow the Topic
-
BMC Musculoskeletal Disorders

BMC Musculoskeletal Disorders is an open access, peer-reviewed journal that considers articles on all aspects of the prevention, diagnosis and management of musculoskeletal disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
Related Collections
With Collections, you can get published faster and increase your visibility.
Diagnostic imaging in musculoskeletal disorders
BMC Musculoskeletal Disorders is calling for submissions to our Diagnostic imaging in musculoskeletal disorders Collection. Accurate and early diagnosis is essential to the effective treatment and management of musculoskeletal disorders. Diagnostic imaging has evolved rapidly, with innovations in MRI, CT, ultrasound, PET, and advanced image analysis techniques—including AI-assisted interpretation—transforming clinical practice and research. This Collection invites research, clinical studies, systematic reviews, and technical innovations that highlight the role of diagnostic imaging in the detection, monitoring, and prognostic evaluation of musculoskeletal conditions. Submissions demonstrating methodological rigor, validation, reproducibility, and clear clinical or translational relevance are particularly encouraged.
Topics of interest include, but are not limited to:
Advancements in imaging musculoskeletal techniques (e.g., high-resolution MRI, dynamic ultrasound, dual-energy CT)
Imaging biomarkers for early diagnosis and disease progression in musculoskeletal disorders, including prognostic and predictive imaging markers
AI and machine learning applications in musculoskeletal imaging with external validation, clinical integration, and outcome prediction
Comparative studies on imaging modalities for specific musculoskeletal pathologies and their influence on clinical decision-making
Quantitative musculoskeletal imaging analysis and its clinical relevance, including radiomics and advanced image-derived biomarkers
Imaging-guided musculoskeletal interventions and minimally invasive procedures
Imaging in musculoskeletal sports injuries and rehabilitation monitoring, including return-to-activity and functional recovery assessment
Standardization, reproducibility, and inter-observer reliability in imaging assessments, including multicenter and external validation studies
Pediatric and geriatric imaging in musculoskeletal disorders
Cost-effectiveness and accessibility of advanced musculoskeletal imaging in clinical settings and value-based imaging approaches across diverse healthcare systems
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Sep 22, 2026
Environmental impacts on musculoskeletal health
BMC Musculoskeletal Disorders is calling for submissions to the Environmental impacts on musculoskeletal health collection. The Collection covers a broad range of topics related to the environmental impacts on musculoskeletal health, addressing both workplace and broader environmental factors that influence bone health and musculoskeletal diseases. Key areas of focus will include the relationship between environmental exposures and bone mineral density (BMD), as well as how poor working conditions—such as prolonged sitting, repetitive motions, and inadequate ergonomic setups—can contribute to musculoskeletal pain and disorders. The collection will also explore how occupational stress, physical strain, and environmental toxins can lead to an increased risk of fractures and musculoskeletal diseases. Additionally, it will cover emerging research on the role of ergonomic workspaces in preventing or mitigating musculoskeletal issues, emphasizing best practices for improving work environments to promote optimal musculoskeletal health.
Topics of interest include, but are not limited to:
Occupational and ergonomic exposures contributing to musculoskeletal disorders
Urbanization, physical inactivity, and access to green space as determinants of musculoskeletal health
Environmental influences on childhood skeletal development or age-related degeneration
Interactions between nutrition, environmental toxins, and bone metabolism
Geographic and socioeconomic disparities in environmental musculoskeletal risk
Policy, prevention, and public health strategies targeting environmental contributors to MSK disease.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 17, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in