The burden of cancer has increased in old people with type 2 diabetes, and inequalities persist
Published in Cancer

Introduction
In the past, the medical community recognised that reducing the risk of cardiovascular complications was paramount in managing and treating diabetes, a chronic metabolic disorder affecting more than 500 million individuals worldwide. Over time, awareness and mass screening in high-income countries, including England, led to earlier detection of diabetes, enabling healthcare providers to implement preventive measures earlier. Combined with advances in drug development for cardiometabolic diseases, the lives of those affected have been prolonged in recent years.
Observational studies and comprehensive meta-analyses have reported an association between diabetes and an increased risk of certain cancers, including pancreatic, liver, and bladder cancer. The scientific community believes this association is because diabetes and cancer share common contributors to their development, such as obesity, physical inactivity, and a poor diet or lifestyle choices, but it could also be due to prolonged exposure to insulin resistance, chronic inflammation, and hyperglycaemia, as people with diabetes are living longer with the disease, owing to implementation of successful cardiovascular prevention strategies over the last few decades.
While previous studies reported a decline in cardiovascular mortality rates among individuals with diabetes, the situation concerning cancer remained unclear. Moreover, within the realm of diabetes-related complications, evidence emerged suggesting that individuals from socially deprived backgrounds faced a higher risk of cardiovascular issues. However, whether similar disparities extended to the realm of cancer remained a topic of uncertainty, requiring further exploration.
What did we investigate?
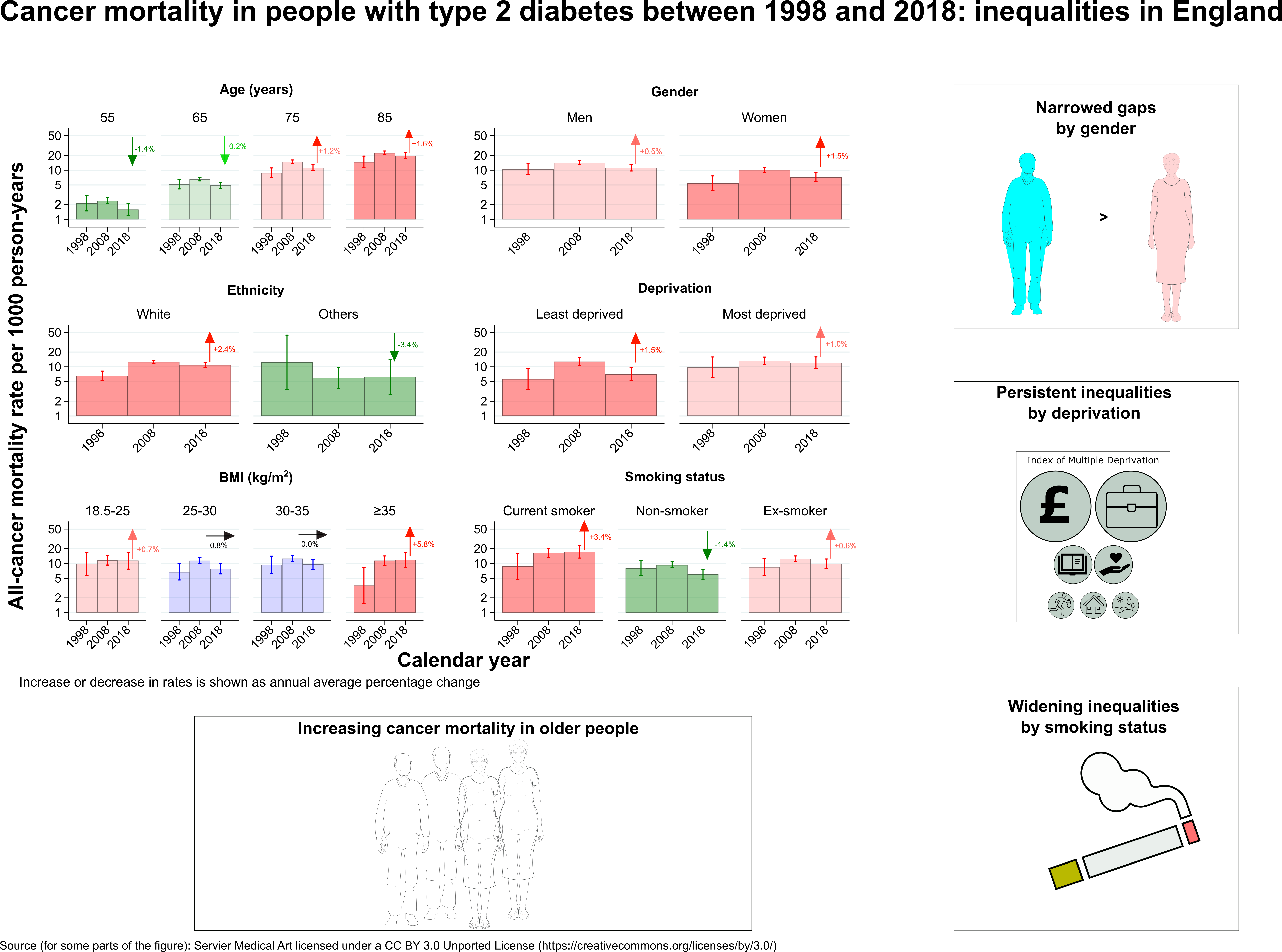
In our study, we included individuals diagnosed with type 2 diabetes using the CPRD, a primary care database comprising more than 400 practices in the UK. To determine the causes of death, we linked this database to the death registration in England. We calculated standardized mortality ratios (SMRs) for cancer in this population, comparing it to the general population in England. We analysed data from 1998 to 2018 and plotted age-specific mortality rates for all causes, all cancers, as well as eight specific cancer types (four commonest: breast, prostate, colorectal and lung; four diabetes-related: pancreatic, liver, gallbladder and endometrial). By quantifying average annual percentage changes in mortality trends, we aimed to understand how these rates evolved over time. To investigate potential inequalities, we further stratified our analyses by sex, ethnicity, deprivation, smoking status, and obesity (body mass index groups). This allowed us to explore whether disparities in mortality rates existed among different subgroups within the type 2 diabetes population.
What did we find?
Our study confirmed that individuals with type 2 diabetes face almost a 20% higher risk of dying from cancer compared to the general population. While overall mortality rates have been decreasing for people with type 2 diabetes of all ages, the rates of cancer-related deaths have been increasing among older individuals (above 65 years). Our findings also revealed persistent disparities in cancer mortality trends based on gender and socioeconomic status, with the gap widening particularly between smokers and non-smokers. Furthermore, we observed an upward trend in pancreatic, liver, colorectal, breast, prostate, lung, and endometrial cancer cases at different ages among those with type 2 diabetes. These findings emphasize the importance of addressing the increased cancer risk associated with type 2 diabetes, particularly among older individuals, and the need to address disparities based on gender, socioeconomic status, and smoking habits.
Why these findings are important?
Our study findings emphasize the importance of giving cancer the same level of attention as other complications, such as cardiovascular and renal diseases, in people with type 2 diabetes. It is crucial to recognize that cancer poses a significant threat to this population and warrants equal prioritisation in healthcare strategies. Future public health research should focus on implementing targeted cancer prevention, early detection, and screening strategies specifically tailored to individuals with type 2 diabetes. These strategies should take into account factors such as gender, socioeconomic status, and smoking habits to ensure that access to cancer prevention, screening and early diagnosis measures is equitable across all groups. By doing so, we can reduce the persistent and widening inequalities observed in cancer mortality trends. Additionally, efforts should be made to raise awareness among healthcare professionals and the general public about the increased cancer risk in individuals with type 2 diabetes, as well as the importance of lifestyle modifications to reduce this risk. Healthcare systems in high-income countries, such as National Health Service England, need to be prepared to see more patients with co-existing diabetes and cancer.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in