The Essential Role of Occupational Therapy for Individuals with Severe Mental Disorder: Insights from Our Scoping Review
Published in Healthcare & Nursing
Why Occupational Therapy Matters in Severe Mental Disorder
Occupational therapy focuses on enabling individuals to engage in meaningful and purposeful daily activities—those that shape identity, structure routines, and contribute to wellbeing. For people diagnosed with a severe mental disorder, the challenges often extend beyond symptom management. Difficulties with social participation, cognitive functioning, motivation, self-care, employment, and daily routines are common and significantly impact quality of life.
Our review revealed that occupational therapy interventions directly target these areas by restoring functional abilities, promoting community participation, and helping individuals build routines that provide stability and meaning. This holistic approach is especially important in severe mental disorder, where long-term recovery depends not only on clinical improvement but also on regaining autonomy and reconnecting with everyday life.
What We Found: Four Main Types of Interventions
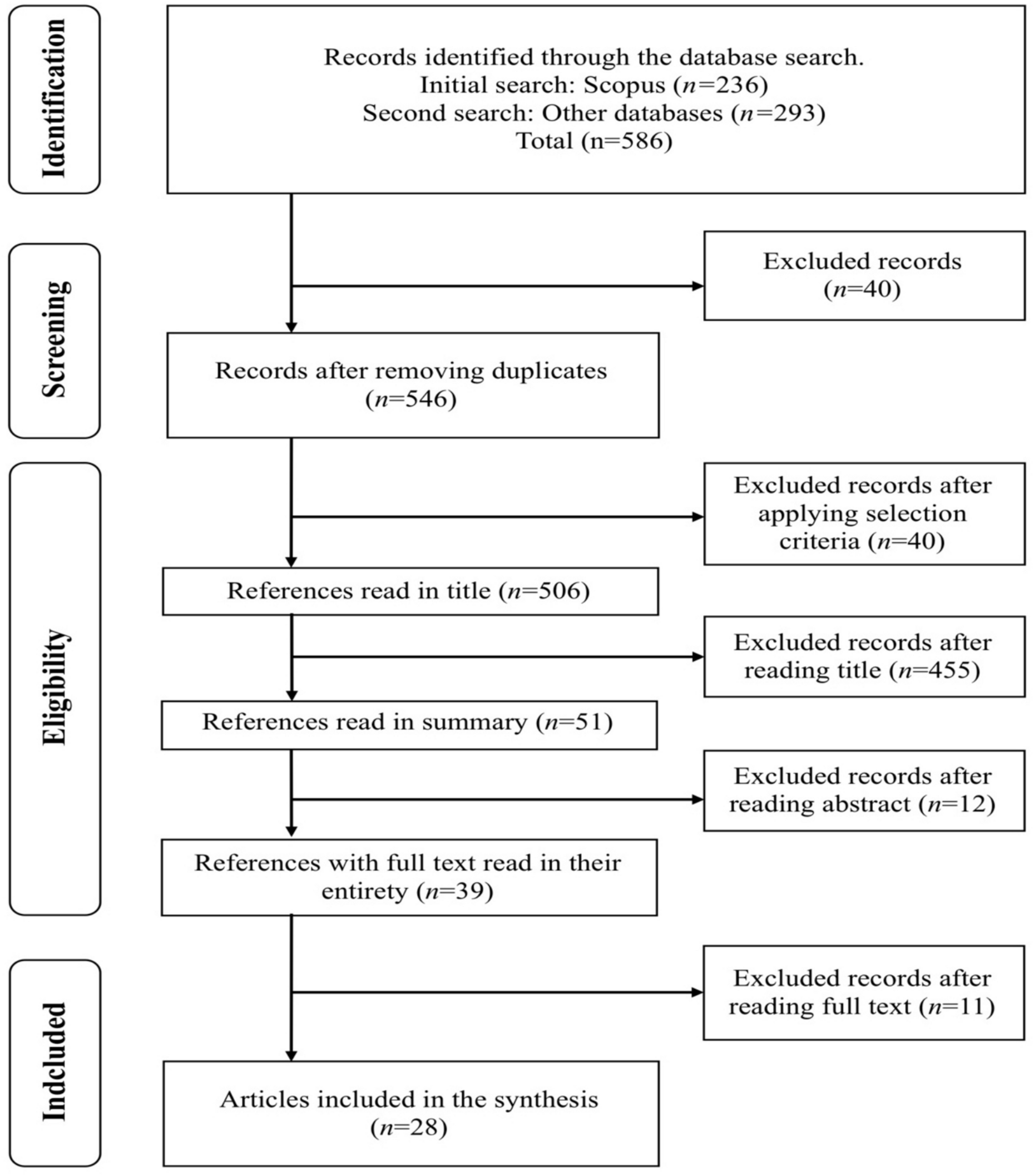
Through an extensive search across multiple databases, our scoping review included 35 eligible studies examining occupational therapy interventions for adults with severe mental disorder. These interventions were grouped into four main categories:
Psychosocial Interventions
These were the most frequently reported. Psychosocial programs often aim to strengthen social skills, increase community participation, and promote engagement in meaningful activities. Many of these interventions are delivered in group settings, with sessions typically lasting around 60 minutes and occurring two to three times per week over several months. The group context fosters social interaction, mutual support, and the development of shared routines—elements particularly beneficial for individuals with severe mental disorder.
Psychoeducational Interventions
These interventions focus on providing knowledge, developing coping strategies, and fostering self-management. By increasing understanding of one’s condition, symptoms, and daily challenges, psychoeducational occupational therapy empowers individuals to make informed decisions and actively participate in their recovery process.
Cognitive Interventions
Cognitive difficulties—such as impairments in memory, attention, or executive functioning—are common in severe mental disorder and can significantly restrict participation in daily occupations. Cognitive-based occupational therapy interventions included exercises for cognitive rehabilitation, cognitive stimulation, and training in functions essential for independent living. These interventions help translate cognitive gains into practical improvements in everyday tasks.
Physical Activity or Exercise-Based Interventions
Incorporating structured physical activity into occupational therapy programs enhances not only physical health but also motivation, emotional regulation, and self-esteem. Our review found that exercise-based occupational therapy is increasingly recognized as a supportive pathway for improving overall functioning in individuals with severe mental disorder.
These categories highlight the flexibility and adaptability of occupational therapy. They also demonstrate how occupational therapists tailor interventions to address the complex and multidimensional needs of this population.
The Value of Group-Based Interventions and Interdisciplinary Collaboration
A striking pattern across the included studies was the predominance of group-based occupational therapy interventions. Group settings provide opportunities for safe social interaction, peer learning, and shared experience—factors essential for individuals who may struggle with isolation, low confidence, or limited social networks.
Additionally, most occupational therapy interventions were implemented within interdisciplinary teams, involving collaboration among psychiatrists, psychologists, nurses, social workers, and other professionals. This collaborative approach ensures a more comprehensive rehabilitation process and reflects best practices in contemporary mental health care.
Benefits Identified in the Literature
Our review shows that occupational therapy contributes meaningfully to recovery across several domains:
-
Autonomy and Self-Care: Occupational therapy interventions help individuals develop, regain, or maintain essential skills for daily living, from personal hygiene to time management.
-
Social Participation: By supporting interpersonal skills and community engagement, occupational therapy reduces isolation and strengthens the sense of belonging.
-
Cognitive Functioning: Cognitive interventions improve foundational skills that allow individuals to function more independently in daily activities.
-
Emotional Wellbeing: Psychoeducational and activity-based interventions promote motivation, self-efficacy, and emotional stability.
Collectively, these outcomes demonstrate that occupational therapy is not merely complementary but fundamental in achieving holistic recovery.
Gaps and Future Directions
Despite promising results, our review also identified notable gaps. Many studies had small sample sizes, heterogeneous methodologies, and limited follow-up periods. More rigorous research is required, including controlled trials, standardized assessment tools, and longitudinal evaluation. Furthermore, while many studies focused on people with schizophrenia, less evidence is available for other diagnostic groups within severe mental disorder.
Future research should also examine how occupational therapy interventions can be adapted for different cultural contexts, diverse communities, and varying levels of functional ability.
Conclusion
Our review reinforces that occupational therapy plays a vital and irreplaceable role in supporting individuals with severe mental disorder. By promoting participation in meaningful activities, strengthening autonomy, and enhancing wellbeing, occupational therapy contributes directly to long-term recovery and social inclusion.
To deliver genuinely person-centred mental health care, healthcare systems must recognize and integrate the unique contributions of occupational therapy. Investing in evidence-based occupational therapy interventions is not only clinically effective but also an essential step toward building more inclusive, humane, and recovery-oriented mental health services.
Authors and Affiliations
Miguel-Ángel Talavera-Valverde, PhD, MSc, OT
Occupational therapist and researcher at the University of A Coruña (UDC), affiliated with the INTEGRA Saúde research group. His work focuses on occupational therapy in mental health, occupational participation and performance, and professional reasoning. He combines teaching activities with clinical practice in the public health system.
Andrea Pérez Ben, OT.
Occupational therapist specializing in mental health interventions.
Ana-Isabel Souto-Gómez, PhD, MSc, SW, OT
Researcher and lecturer in occupational therapy at the University of Santiago de Compostela (Escola Universitaria de Traballo Social), also affiliated with INTEGRA Saúde. Her work focuses on professional identity, the development of inclusive communities from a social work perspective, and occupational therapy interventions in mental health. She has actively participated in studies on professional practice and pre- and postgraduate training in social work and occupational therapy.
Follow the Topic
-
Journal of Psychosocial Rehabilitation and Mental Health

Journal of Psychosocial Rehabilitation and Mental Health is a multidisciplinary journal that emphasizes recovery-oriented care and rehabilitation in mental health.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Thank you