World Pneumonia Day 2025: The Global Burden of a Persistent and Preventable Threat
Published in Sustainability, General & Internal Medicine, and Education
About the Researcher
Dr . Catia Cillóniz is the Coordinator of the Research Line in Pneumonia within the Research Group of Applied Research in Infectious Respiratory Diseases and Critically Ill Patients at IDIBAPS. She also serves as the Coordinator of the Worldwide Pneumonia Awareness Campaign – Pneumolight. Dr. Cilloniz is a Fellow of the European Respiratory Society (ERS) and Secretary of the Tuberculosis and Respiratory Infections (TIR) Area of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). She is also a member of the Advisory Group for the Assembly on Pulmonary Infections and Tuberculosis (PI-TB) of the American Thoracic Society (ATS). She is co-guest editor for an open collection, “Corticosteroids in Pneumonia and Critical Illness: Precision, Practice, and Progress”, in the Pneumonia journal.
Global Impact of Pneumonia
According to the recently published Global Burden of Disease report, pneumonia claimed 2.5 million lives worldwide in 2023, representing a 19% increase compared to 2021 (2.1 million deaths)[1]. Children under five remain among the most vulnerable populations, accounting for nearly a quarter of all deaths (600,000), while adults aged 70 years and older represented almost half (1.2 million). Together, these two groups made up 70% of all pneumonia deaths globally[1].
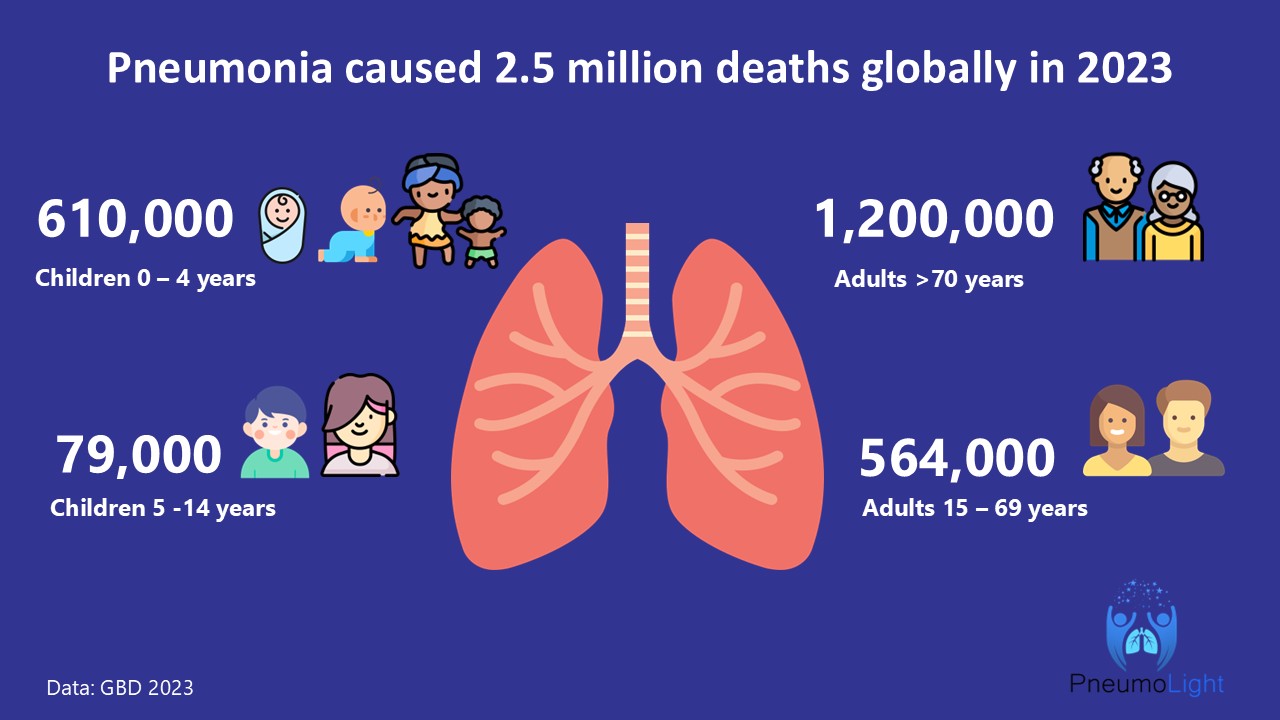
The highest burden was reported in Sub-Saharan Africa and across South and East Asia and the Pacific, which together accounted for 68% of all pneumonia deaths in 2023[1]. These data highlight persistent inequities in prevention and access to life-saving interventions such as antibiotics and therapeutic oxygen.
Every year, November 12 marks World Pneumonia Day, a call to action for all of us to unite against this global yet largely preventable and treatable disease. Coordinated efforts among researchers, clinicians, public health authorities, policymakers, and communities are urgently needed to reduce the burden of pneumonia and prevent unnecessary deaths.
We live in an era of unprecedented scientific advancement—discussing omics, personalized medicine, and cutting-edge therapeutics. Yet, despite these innovations, the impact of pneumonia remains profound, as access to these advances is limited to a privileged few. Inequality continues to be one of the greatest barriers to global health equity, and it goes against our achievement of universal health coverege: one of UN’s Sutainable Development Goals, namely target 3.8.
Over the past few decades, we have also observed significant changes in the epidemiology of pneumonia. There is a growing proportion of vulnerable individuals, including older adults with chronic comorbidities and immunosuppressed patients, which poses new challenges for management.
Another notable shift has been our understanding of respiratory viruses. Before the COVID-19 pandemic, their role in pneumonia was often underappreciated. Now, with routine testing for respiratory viruses, we better understand their contribution—not only in the acute phase and related complications such as cardiac events, but also in the long-term sequelae, including cardiac and neurological complications. This evolving knowledge has transformed our perception of viral pneumonia and its broader implications for global health.
Finally, the rise of antimicrobial resistance (AMR) adds another layer of complexity. The 2021 Global Burden of Disease report estimated that 4.71 million deaths were associated with bacterial AMR[2], including 1.14 million directly attributable to it. Addressing AMR must be a central component of global pneumonia control strategies, and it is essential to achieve SDG3 and for promoting health and well-being for all.
Reducing the Global Burden of Pneumonia
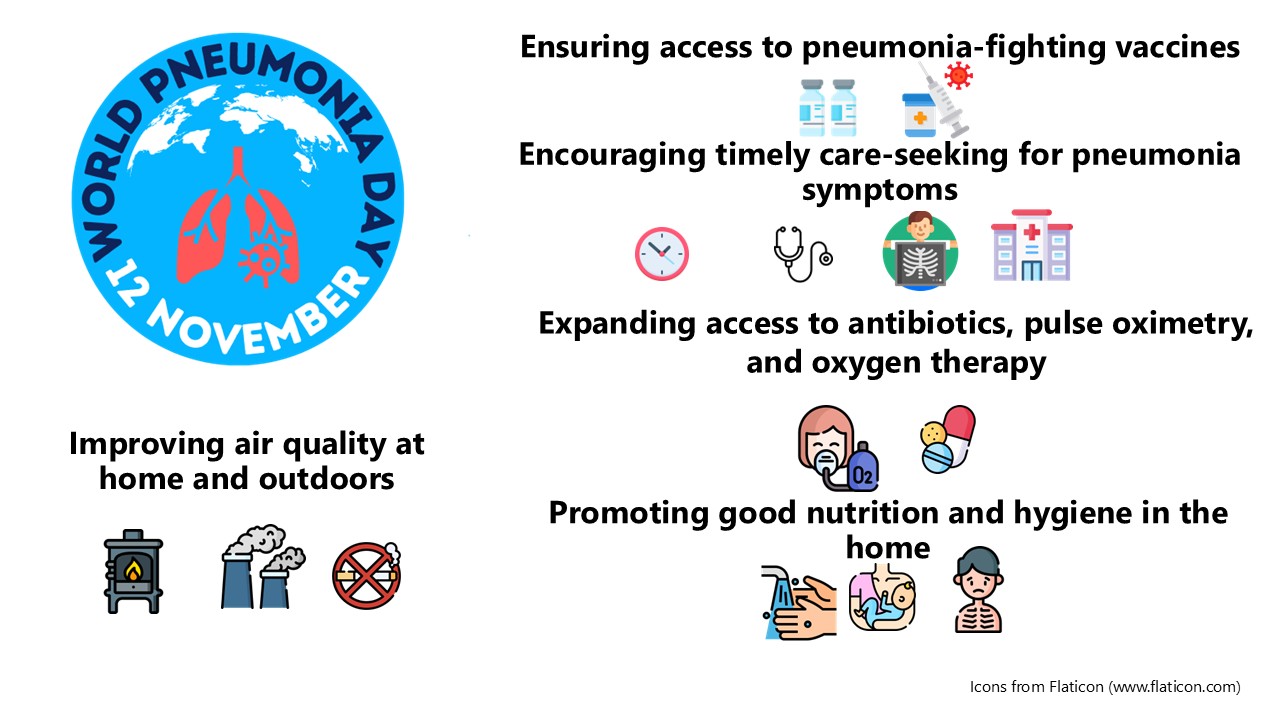
The burden of pneumonia can be substantially reduced through increased access to life-saving pneumonia interventions. The following actions are essential:
1.-Ensuring access to pneumonia-fighting vaccines
Vaccines remain the most effective intervention for preventing pneumonia deaths. These include the pneumococcal conjugate vaccine (PCV), Haemophilus influenzae type B (Hib) vaccine, diphtheria-tetanus-pertussis (DTP), measles (MCV), influenza, respiratory syncytial virus (RSV), and COVID-19 vaccines.
According to a study published in 2019, nearly 400,000 of the 672,000 annual child deaths from pneumonia could be prevented through pneumococcal vaccination alone, and 54.6 million pneumonia episodes could be averted each year[3].
Efforts must focus on supporting vaccine introduction and implementation, while ensuring affordable access for disadvantaged and vulnerable populations.
2.-Improving air quality at home and outdoors
Exposure to air pollution and smoking are leading risk factors for pneumonia-related deaths. 2.4 billion people worldwide still lack access to clean cooking. The World Health Organization estimated that household air pollution caused 3.2 million deaths annually in 2020, including over 237,000 deaths among children under five[4]. In 2019, 749,000 deaths were linked to air pollution from household and outdoor sources combined[5, 6].
Implementing policies to reduce air pollution is critical to lowering pneumonia mortality.
3.-Promoting good nutrition and hygiene in the home
Proper nutrition and hygiene are key to pneumonia prevention. Exclusive breastfeeding for the first six months of life protects infants from infectious diseases, yet 52% of infants aged 0–5 months globally are not exclusively breastfed[7]. Breastfeeding provides essential immune protection that reduces the risk of pneumonia and other infections.
In addition, access to handwashing with soap is vital to preventing the spread of respiratory pathogens. A lack of handwashing facilities contributes to approximately 270,000 pneumonia deaths globally[6].
4.-Encouraging timely care-seeking for pneumonia symptoms
Early care-seeking for children with pneumonia symptoms significantly reduces mortality. However, 44% of children with pneumonia symptoms worldwide are not taken to a qualified healthcare provider. In Sub-Saharan Africa, where pneumonia deaths are highest, only 45% of children with acute respiratory infection symptoms receive care, with even lower rates in rural areas (43%).
Education and awareness campaigns are essential to promote prompt care-seeking behavior and ensure children receive appropriate treatment.
5.-Expanding access to antibiotics, pulse oximetry, and oxygen therapy
Healthcare facilities must be equipped with pulse oximeters to detect hypoxemia and administer oxygen when necessary. Early detection of hypoxemia in severe pneumonia is crucial for reducing mortality. Expanding the use of pulse oximetry in high-burden countries, along with training for health workers, can save countless lives[8].
Oxygen therapy remains a cornerstone of treatment for severe pneumonia and should be made universally accessible.
Preventing and treating pneumonia is critical to advancing the UN’s Sustainable Development Goals, especially SDG 3 on good health and well-being. By increasing access to vaccines and healthcare, we move closer to universal health coverage and lower child mortality worldwide
Raise Awareness
On November 12, as part of the Worldwide Pneumonia Awareness Campaign-Pneumolight, we will host the 5th Global Conference for World Pneumonia Day, a free hybrid event bringing together leading experts and organizations in global health, infectious diseases, and respiratory medicine.
This year’s theme — “Enhancing Diagnosis, Managing Oxygen Needs, and Tackling Antibiotic Resistance” — highlights critical scientific and clinical priorities to reduce pneumonia mortality worldwide. The conference will feature presentations on innovations in pneumonia diagnosis, equitable access to oxygen therapy, and strategies to combat antimicrobial resistance, as well as discussions on vaccines, respiratory virus threats, and international partnerships for pneumonia prevention and care.
You can register and view the full program through the following: https://pneumolightconference.com/
Access free infographics and shareable videos to help raise awareness about pneumonia here: https://pneumolightconference.com/toolkits/
For more related events and activities for World Pneumonia Day, you can explore them here: https://stoppneumonia.org/latest/world-pneumonia-day/

Scientific Research
There is an open collection, “Corticosteroids in Pneumonia and Critical Illness: Precision, Practice, and Progress”, in the Pneumonia journal, compiling current research on corticosteroid therapy, clinical practice insights, and emerging evidence in severe pneumonia and critical illness. Submit your articles to contribute to this ongoing collection.
References
1 GBD 2023 Causes of Death Collaborators. Global burden of 292 causes of death in 204 countries and territories and 660 subnational locations, 1990-2023: a systematic analysis for the Global Burden of Disease Study 2023. Lancet 2025; 406: 1811–1872.
2 Naghavi M, Vollset SE, Ikuta KS, et al. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. The Lancet Elsevier; 2024; 404: 1199–1226.
3 Chen C, Cervero Liceras F, Flasche S, et al. Effect and cost-effectiveness of pneumococcal conjugate vaccination: a global modelling analysis. Lancet Glob Health 2019; 7: e58–e67.
4 Household air pollution [Internet]. [cited 2025 Oct 23]. Available from: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health.
5 Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Elsevier; 2020; 396: 1204–1222.
6 JustActions. The Missing Piece. Why the global pandemic is an inflection point for pneumonia control. Revised and updated for COVID-19 and the Global Burden of Disease 2019. New York, USA. 2021.
7 Breastfeeding [Internet]. UNICEF DATA [cited 2025 Oct 23]. Available from: https://data.unicef.org/topic/nutrition/breastfeeding/.
8 Cilloniz C, Simonds A, Hansen K, et al. Pulse oximetry is an essential tool that saves lives: a call for standardisation. Eur Respir J 2021; 57: 2100815.
Follow the Topic
-
Pneumonia

This journal is the only journal to focus exclusively on pneumonia. It provides an international forum for the exchange of knowledge by scientists and clinicians involved in studying the etiology and pathogenesis of pneumonia, as well as its diagnosis, epidemiology, treatment and prevention.
Your space to connect: The Primary immunodeficiency disorders Hub
A new Communities’ space to connect, collaborate, and explore research on Clinical Medicine, Immunology, and Diseases!
Continue reading announcement
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in