The Southern European Atlantic diet and depression risk
Published in Healthcare & Nursing

The Southern European Atlantic diet (SEAD) is the traditional diet of north-western Spain and northern Portugal. It comprises cod, other fresh fish, red meat and pork products, dairy, legumes and vegetables, vegetable soup, potatoes, whole-grain bread, and wine.
While the consumption of red meat, pork products, and potatoes is partially inconsistent with current healthy dietary recommendations, increased adherence to the SEAD has been associated with healthier gut microbiota, reduced levels of several cardiovascular risk factors, and decreased risk of myocardial infarction and all-cause mortality. Nevertheless, existing healthy dietary patterns may also play a favourable role in mental health conditions, while associations with the SEAD were uncertain.
In this study, we examined the association between adherence to the SEAD and depression risk in 13,297 participants from Spain, Czechia, Poland, and the United Kingdom, who were followed-up for 3.9 years on average. Using logistic regression models adjusted for sociodemographic, lifestyle, and dietary variables, we found an association between higher adherence to the SEAD and lower depression risk (Figure 1).
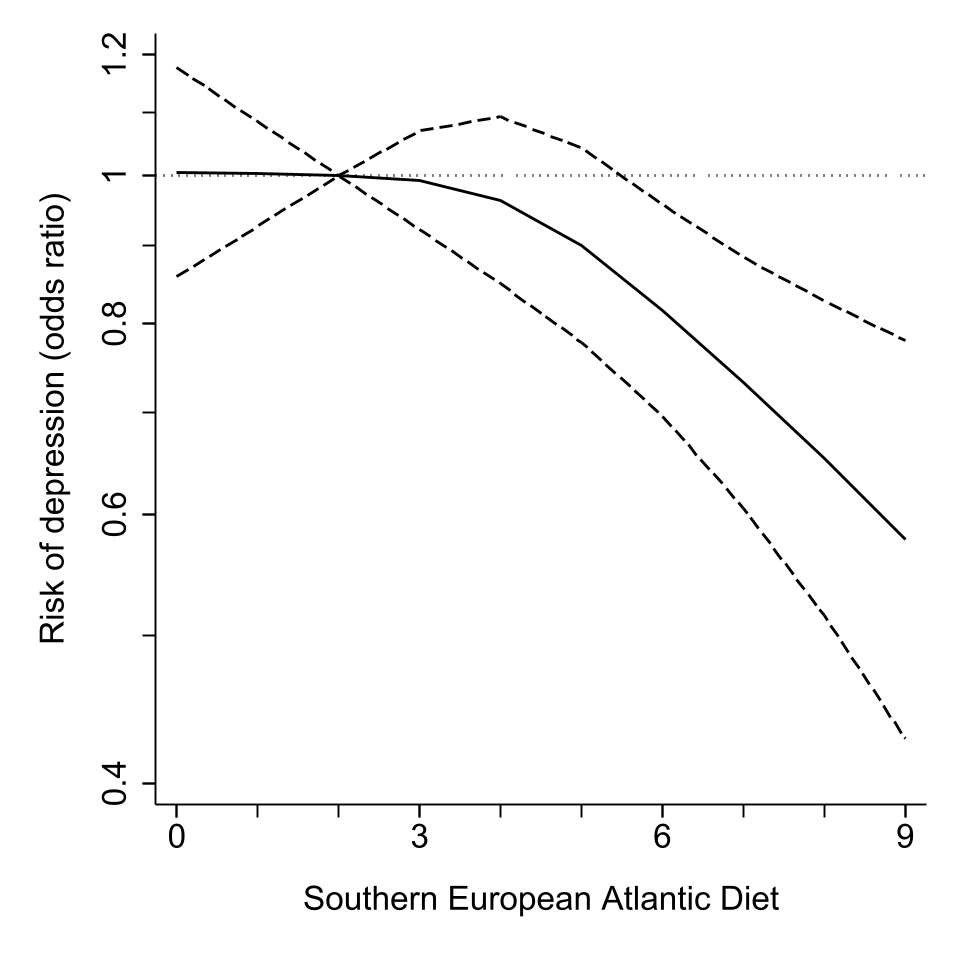
Figure 1. Odds ratios (95% confidence interval) of the association between adherence to the Southern European Atlantic diet and 3.9-year risk of depression.
Most individual food groups showed similar tendencies, albeit non-significant and weaker than that of the SEAD as a whole. This is not surprising, as dietary patterns can account for the small cumulative effects of food groups on chronic disease risk and for complex interactions between nutrients. In other words, the whole is not the same as the sum of its parts.
The association of the SEAD with lower depression risk was rather consistent across countries and of similar magnitude as that found for the Mediterranean diet and the Alternative Healthy Eating Index. This implies that different diets could confer comparable benefits on depression risk.
Several limitations should be acknowledged. First, food consumption was self-reported, and no dietary data were collected in the follow-up waves. Second, depression assessment differed across cohorts, and some depression cases were likely missed because of the rather long intervals between data collection. Third, there is potential for residual confounding, as several variables were likely measured with some error, and some potential confounders could not be accounted for.
In conclusion, the SEAD was associated with lower depression risk across European populations. This may support the development of mood disorder guidelines for Southern European Atlantic regions based on their traditional diet, and for central, eastern, and western European populations based on the SEAD food groups that are culturally rooted in these places.
We thank the participants, researchers, and support staff of the Seniors-ENRICA-1, Seniors-ENRICA-2, HAPIEE, and Whitehall-II studies, who made our research possible.
Follow the Topic
-
Molecular Psychiatry

This journal publishes work aimed at elucidating biological mechanisms underlying psychiatric disorders and their treatment, with emphasis on studies at the interface of pre-clinical and clinical research.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in