Towards a Safe Treatment of Eye Floaters by Light-Induced Vapor Nanobubbles
Published in Healthcare & Nursing
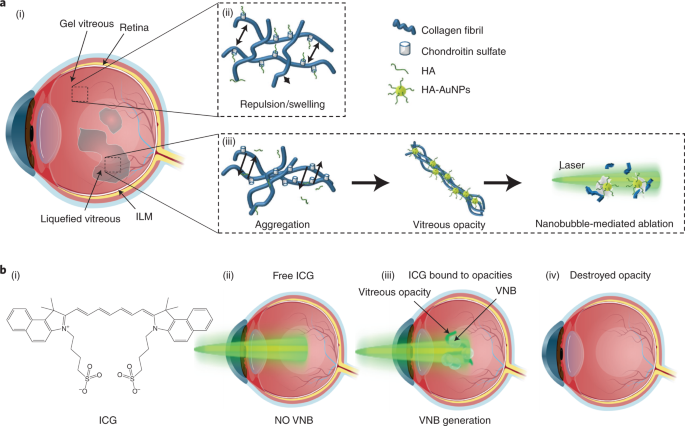
The vitreous of the eye is a transparent gel mainly composed of water, glycosaminoglycans and a network of collagen fibrils. In healthy eyes, collagen fibrils are spaced apart by hyaluronic acid (HA), an anionic glycosaminoglycan which attracts water and generates a swelling pressure that inflates the gel to maintain its transparency. Vitreous collagen fibrils are heterotypic in composition. They contain collagen type II, V, IX and XI. Type IX collagen has chondroitin sulfate glycosaminoglycan chains which extend away from the fibril surfaces; they space apart the collagen fibrils, thereby preventing the aggregation of collagen fibrils. With aging, myopia or diabetes, there is a progressive ‘liquefaction’ of the vitreous inducing the formation of collagen aggregates that scatter light and can strongly impact vision and quality of life.
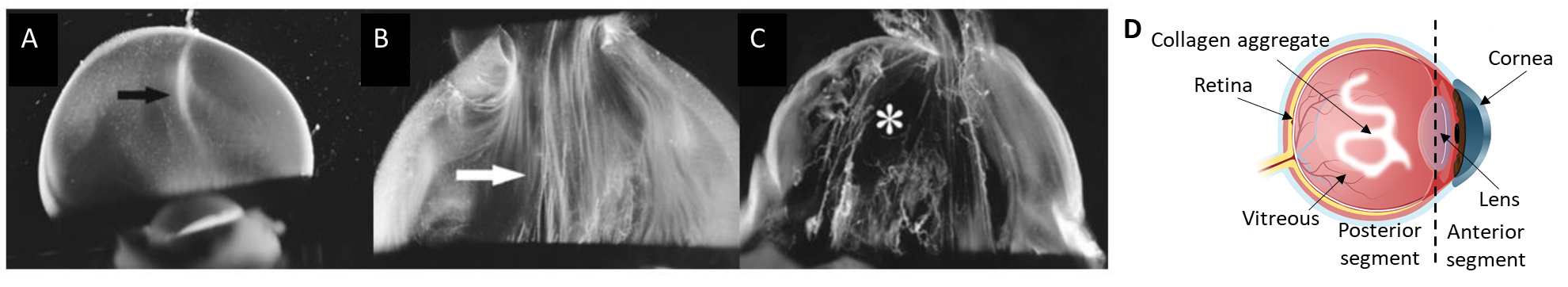
Figure 1. Dark-field slit microscopy of dissected human vitreous body reveals aging structure. (A) Homogeneous vitreous of a 33-week old fetus. (B) Fusion of collagen fibrils in the central part of the vitreous (white arrow) of an 59-year-old human. (C) Extensive fibrous liquefaction in the degenerated vitreous of an 88-year-old woman. This degeneration is accelerated in myopia and simultaneously forms vitreous opacities (D)1.
In most cases, vitreous opacities are left untreated and patients must cope with at times debilitating symptoms. While vitrectomy (i.e. surgical excision of vitreous) is currently performed to cure eye floaters, it is invasive, costly, and carries risks. Laser treatment has unproven efficacy and remains rather limited because vitreous opacities have to be located sufficiently far from the retina to avoid photomechanical collateral damage. Thus, an approach to increase patient eligibility and reduce laser intensity would meet an unmet medical need.
Exploiting the plasmonic properties of gold nanoparticles, surrounding water evaporates when illuminated with a pulsed-laser, forming ‘vapor nanobubbles’ (VNBs). In 2019, we reported that when nanobubbles collapse, the accompanying mechanical forces destroy vitreous opacities onto which gold nanoparticles are bound.2 This was achieved with a laser fluence 1000 times lower than currently used clinically. These in vitro and ex vivo studies showed proof of principle requiring corroboration in vivo, but no experimental model existed.
For the first time, we demonstrate safe destruction of vitreous opacities in live rabbits using gold nanoparticles as well as indocyanine green (ICG), a dye which is clinically used in ophthalmology for choroidal angiography3 and chromodissection.4 We observed in situ preferential binding to vitreous opacities that were previously obtained from patients during vitrectomy. VNBs were generated in a targeted fashion due to preferential accumulation on the surface of the opacities, thus leaving the surrounding vitreous untouched. In rabbits, it was observed that both gold nanoparticles and ICG were well tolerated and destroyed opacities after few pulses at 1.9 J/cm²; for ICG, at a lower concentration than used during chromodissection.5
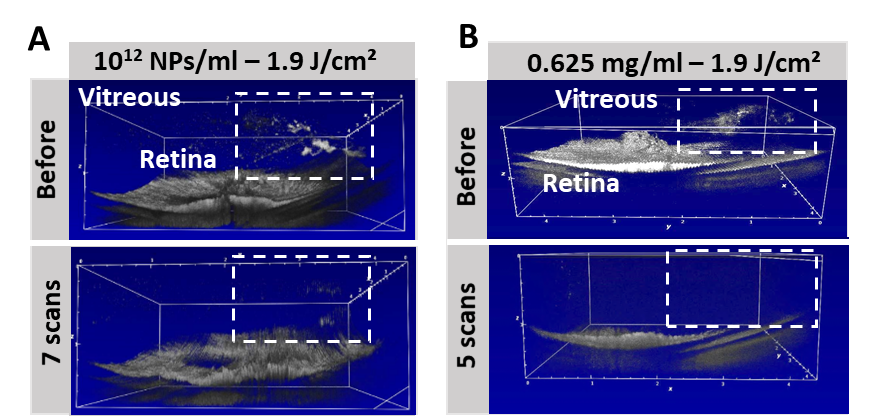
Figure 2 Following (A) gold nanoparticles (1012 NPs/ml) or (B) ICG injection (0.625 mg/mL), laser irradiation (<7ns; 532 nm (gold) or 800 nm (ICG); 1.9 J/cm²) enabled the ablation of exogenous collagen opacities after few pulses.
Importantly, this occurs at a laser energy which is one thousand times less than the (YAG laser) energies typically employed clinically, making this highly attractive for safe treatments. Taken together, these results suggest that VNBs generated from gold nanoparticles or ocular dyes like ICG hold great promise for safe laser ablation of vitreous opacities, curing vision degrading myodesopsia.1 With these encouraging results, we aim at expanding nanobubble-mediated ablation more generally to ocular surgery by further increasing safety and precision.
Félix Sauvage
J. Sebag
Stefaan C. De Smedt
References
- Sebag, J. Vitreous and Vision Degrading Myodesopsia. Progress in Retinal and Eye Research 100847 (2020) doi:10.1016/j.preteyeres.2020.100847.
- Sauvage, F. et al. Photoablation of Human Vitreous Opacities by Light-Induced Vapor Nanobubbles. ACS Nano 13, 8401–8416 (2019).
- Desmettre, T., Devoisselle, J. M. & Mordon, S. Fluorescence Properties and Metabolic Features of Indocyanine Green (ICG) as Related to Angiography. Survey of Ophthalmology 45, 15–27 (2000).
- Burk, S. E., Da Mata, A. P., Snyder, M. E., Rosa, R. H. & Foster, R. E. Indocyanine green-assisted peeling of the retinal internal limiting membrane. Ophthalmology 107, 2010–2014 (2000).
- Haritoglou C, Sebag J: Indications and considerations for chromodissection. Retinal Physician 11:34-39, (2014).
Follow the Topic
-
Nature Nanotechnology

An interdisciplinary journal that publishes papers of the highest quality and significance in all areas of nanoscience and nanotechnology.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in