Understanding “Colon Age”: A New Approach to Colorectal Cancer Screening
Published in Biomedical Research

Because of the growing trend in early-onset colorectal cancer (CRC) among younger populations (1), the U.S. Preventive Services Task Force recently shifted their recommendation from starting CRC screening at age 50 to age 45. There remains a catch: even if uptake of these screening recommendations is high among 45-49 year olds, half of early-onset CRC cases will be missed prior to development of signs and symptoms. It is estimated that around 30-35% of the eligible U.S. population 45-75 years old is not current with screening (2). With the long-term goal of determining who should be considered for early screening, we sought to contribute to improving prevention and early detection of early-onset CRC.
A Closer Look at a High-Risk Group
CRC is the most common cause of visceral cancer death in men younger than age 50 (1). Male veterans, in particular, may be at higher risk for CRC than non-veterans due to differences in lifestyle factors and perhaps certain environmental exposures. To identify specific risk factors for early-onset CRC in this population, we acquired and examined data from the electronic medical records of 600 male Veterans with CRC aged 35 to 49 and compared them to two matched control groups—one based on colonoscopy findings and the other from general clinic visits (3).
We analyzed these data using a split-sample approach: a derivation dataset (used to develop the model) and a validation dataset (used to test it). Following full model analysis, we developed two models – one model with 15 key risk factors, and a simpler one with 7. Both performed well in identifying risk for early-onset CRC. Some “standout” risk factors included: no service-connected disability, higher comorbidity index, family history of CRC, and not using NSAIDs or statins.
Making Risk Relatable
A challenge in clinical and preventive medicine is how to relate risk factors to “risk” for an individual patient. This concept is important for considering not only whom to screen early, but also how. People often relate how “old” they feel or how their body functions relative to their age; we applied this paradigm to CRC screening. We applied our validated 15- and 7-variable models to create a new measure for understanding an individual’s risk for CRC and, by extension, their personalized need for CRC screening (4).
We refer to this metric as “Colon Age”, which indicates the biological age of a person’s colon by combining their individual risk profile with population-based CRC occurrence rates. This is achieved by multiplying a patient’s specific risk factors (as identified in the 15- or 7-variable model) with their Surveillance, Epidemiology and End Results (SEER) age-specific rate. Think of being told, “you have the colon age of a 60-year-old” to someone who is only 45 years old.
What Do Patients and Providers Think?
Colon Age is intended to express a patient’s individual risk for CRC in terms that are relatable. Given the absence of evidence for superiority of any single screening strategy, often primary care providers are relied upon to bring up screening during annual exams. Therefore, we completed two qualitative studies regarding the perceived clinical utility and acceptance of simple CRC risk prediction tools.
Round 1: In interviews with 15 patients and 15 primary care providers, we asked about the facilitators and barriers of a simple five-variable risk prediction model in clinical practice (5). Providers had concerns regarding the tool’s accuracy and consistency with guidelines, but both patients and providers agreed that such a tool would generate discussion about CRC screening in clinic and potentially increase screening uptake.
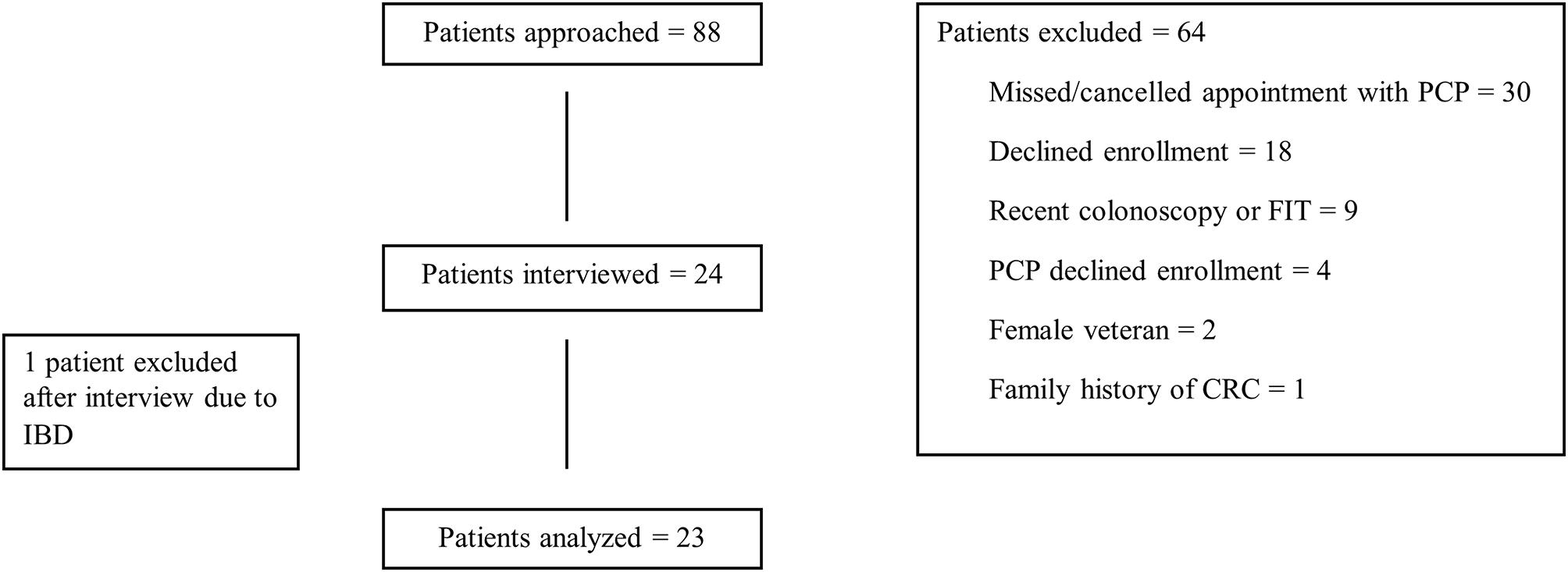
Round 2: We received similar feedback when interviewing 24 patients and 8 primary care providers using the validated 7-variable Colon Age model (6). Patients found the tool easy to understand, as well as empowering in terms of being informed and making their own decisions about CRC screening. Providers agreed that the Colon Age metric may allow greater patient autonomy regarding CRC screening at a time when patients are hesitant to get screened prior to age 50. The Colon Age tool was perceived as a way to get patients involved in their screening decisions, and 96% of the patients we interviewed agreed to have their Colon Age calculated.
There remain some concerns. Time is tight during clinic visits. Some patients were hesitant to share too much personal information, and both groups just wanted to know more about how the tool actually works. Some providers likened the Colon Age tool to the increasingly important concept of precision medicine.
Moving Forward: Precision, Personalization, and Prevention
Despite some limitations, the Colon Age tool appeared to be acceptable and useful to patients and providers in individualizing risk for CRC. It certainly isn’t a silver bullet, but the metric may be a helpful tool for getting high-risk people 45-49 years old screened for CRC (as is currently guideline-recommended) and those younger than age 45 screened sooner, if thought to be clinically appropriate. Colon Age also reflects the growing push toward precision medicine and shared decision-making, two trends that are shaping the future of primary care.
By allowing patients and providers to talk more openly and accurately about individual risk, they can work toward making informed, personalized decisions on when and how to get screened—because catching CRC early can save lives.
References:
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024 Jan;74(1):12–49.
- Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US preventive services taskforce. JAMA. 2016;315(23):2576–94.
- Imperiale TF, Myers LJ, Barker BC, et al. Risk Factors for Early-onset Sporadic Colorectal Cancer in Male Veterans. Cancer Prev Res. 2023;16(9):513–522.
- Imperiale TF, Myers LJ, Barker BC, et al. Colon Age: A Metric for Whether and How to Screen Male Veterans for Early-Onset Colorectal Cancer. Cancer Prev Res. 2024;17(8):377–384.
- Matthias MS & Imperiale TF. A risk prediction tool for colorectal cancer screening: a qualitative study of patient and provider facilitators and barriers. BMC Fam Pract. 2020;21, 43.
- Imperiale TF, Cheng M, Thomas MR et al. A qualitative study of a new metric for estimating early-onset colorectal cancer risk in male veterans: “Colon Age”. BMC Prim. 2025;26, 226.
Follow the Topic
-
BMC Primary Care

Previously known as BMC Family Practice, this is an open access, peer-reviewed journal that considers articles on all aspects of primary health care research.
Related Collections
With Collections, you can get published faster and increase your visibility.
Bridging primary and palliative care
BMC Primary Care is calling for submissions to our Collection, Bridging primary and palliative care. The integration of primary and palliative care is increasingly recognized as essential for improving the quality of life for patients with serious illnesses. This Collection invites research that examines innovative models of care that bridge these two critical domains. The interplay between primary care and palliative care can enhance the patient experience by addressing not only medical needs but also psychosocial and spiritual aspects of care. As healthcare systems evolve, understanding how these two areas can collaborate effectively is crucial for optimizing patient-centered approaches and ensuring comprehensive support for individuals and families.
Advancements in this field highlight the importance of shared decision-making and advanced care planning as mechanisms to enhance communication between healthcare providers and patients. By fostering a collaborative environment, we can empower patients to express their preferences and values concerning their care journey, particularly in the context of end-of-life decisions. Research has shown that integrated approaches lead to better symptom management, reduced hospitalizations, and increased patient and family satisfaction. Ongoing research could transform how we think about and deliver care for patients with serious illnesses.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Integrating advanced care planning in primary care
- Shared decision-making in end-of-life care
- Models of palliative care in primary care settings
- Enhancing communication between care teams
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 08, 2026
Indigenous health and well-being
BMC Primary Care is calling for submissions to our Collection, Indigenous health and well-being. Historically, Indigenous communities have faced significant health disparities driven by systemic inequalities, cultural disconnection, and barriers to accessing healthcare. This Collection seeks to address these issues by gathering research that highlights the unique health challenges faced by Indigenous peoples, including chronic diseases, mental health issues, and the impact of social determinants on health outcomes. By amplifying Indigenous voices and perspectives, we aim to foster a deeper understanding of their health needs and aspirations.
The significance of researching Indigenous health lies in its potential to inform and transform healthcare practices, policies, and systems to achieve health equity. As research grows, we anticipate developments in the field of Indigenous health that may lead to the co-creation of innovative healthcare models. By fostering collaborations between Indigenous communities and healthcare providers, there is potential for enhanced accessibility, culturally appropriate care, and the development of policies that prioritize Indigenous health and well-being. Future studies may also uncover new insights into the role of traditional practices in modern healthcare systems, ultimately bridging the gap between Western medicine and Indigenous healing practices.
In this Collection, we welcome submissions that span a wide array of topics, including but not limited to:
- Barriers to healthcare access for Indigenous populations
- Community health initiatives in Indigenous communities
- Health equity strategies for Indigenous well-being
- Cultural competency in Indigenous healthcare
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 05, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in