Vagus nerve stimulation improves insomnia in breast cancer.
Published in Bioengineering & Biotechnology, Neuroscience, and Biomedical Research

Insomnia and related cancer-related fatigue (CRF) pose a substantial and frequently undertreated crisis for cancer patients, creating a critical unmet health need within oncology care . The incidence of insomnia in cancer patients is estimated to be two to three times greater than in the general population. Women diagnosed with breast cancer are particularly vulnerable, reporting some of the highest prevalence rates of insomnia and fatigue, estimated to range from 38% to 70%. These conditions are not merely discomforts; they are critical concerns linked to poorer treatment outcomes, slower recovery, decreased overall health, and a diminished quality of life. Furthermore, sleep disruption in women with advanced breast cancer has even been identified as a survival predictor.
Current clinical guidelines for chronic insomnia primarily recommend cognitive behavioral therapy for insomnia (CBT-I) or pharmacological interventions. While CBT-I is considered the "gold standard" due to its efficacy and long-lasting effects, its utility is hindered by limited access to qualified providers, uneven geographical distribution of clinics, and poor adherence, with up to 40% of patients dropping out prematurely. Alternatively, pharmaceutical treatments, which often involve sedative-hypnotic agents, are not intended for long-term use due to the risk of physiological dependence and severe adverse effects, including increased risks of depression, cancer, and mortality, concerns that are particularly significant for cancer survivors.
Auricular Bioelectronic Medicine
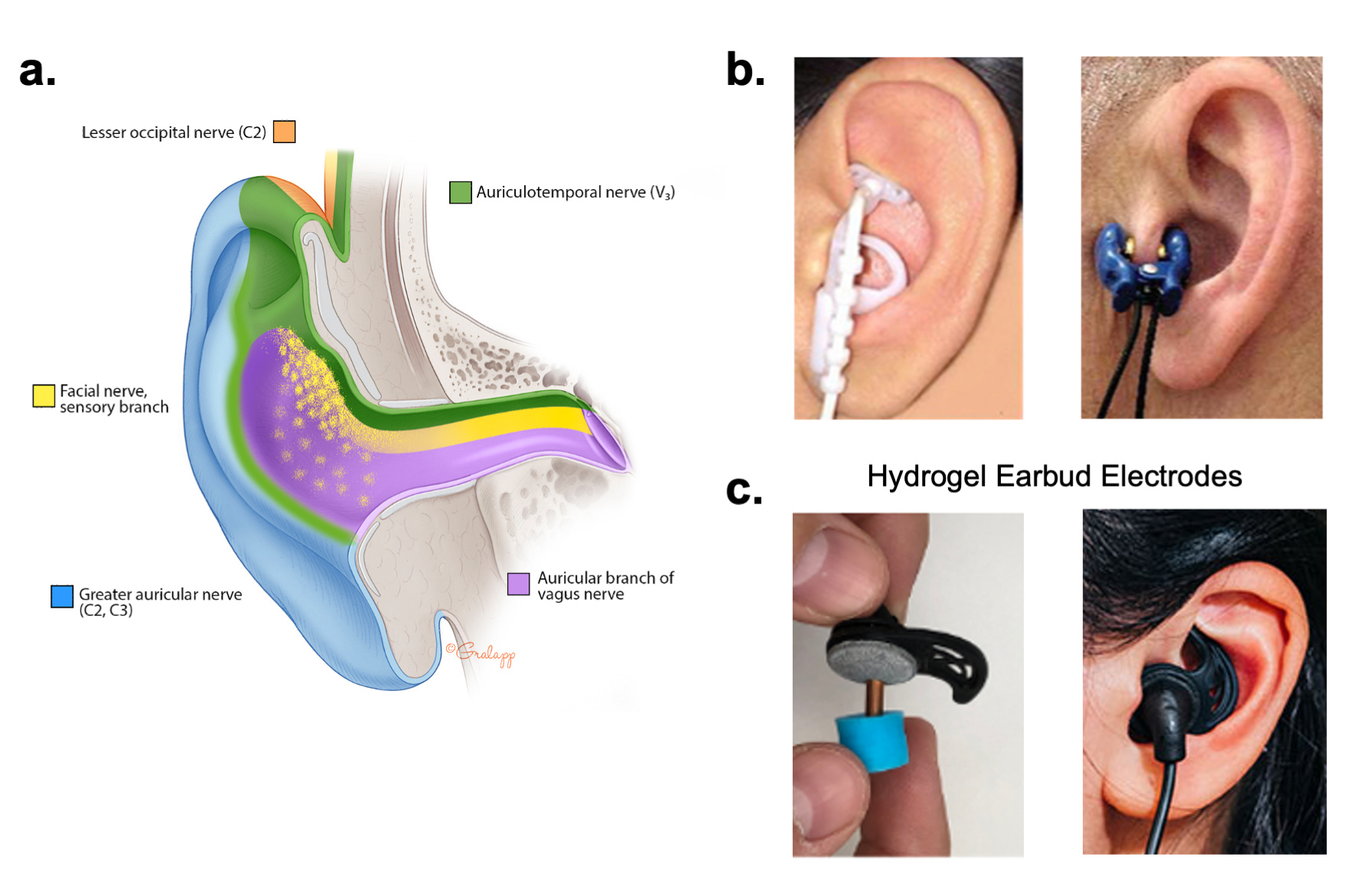
To address the limitations of conventional therapies, we evaluated a non-pharmacological neuromodulation approach known as transcutaneous auricular vagus nerve stimulation (taVNS). This method involves delivering pulsed electrical currents to fibers of the auricular branch of the vagus nerve (ABVN) located in the external acoustic meatus (EAM) of the ear. The study specifically utilized an advanced delivery system called BRAIN Buds, which are comfortable, conductive hydrogel earbud electrodes (Figure 1) [1]. This familiar form factor and advanced electrode design were chosen to improve the electrical efficiency, comfort, usability, scalability, and ease of integration of taVNS methods into routine patient care.
Our open-label pilot clinical trial aimed to evaluate the safety, feasibility, and preliminary efficacy of nightly, bilateral taVNS in women with breast cancer [2]. Twenty female participants, averaging 58.55 years of age, self-administered the taVNS treatment at home for 15 minutes each night for two consecutive weeks. The stimulation intensity was set by the subjects at or just above their sensory threshold, ensuring the sensation was effective yet comfortable.
Safety, Feasibility, and Tolerability
The trial demonstrated that bilateral taVNS was safe, tolerable, and feasible for breast cancer patients. Importantly, no serious adverse events or adverse effects were reported. While some subjects noted mild discomfort that was resolved with proper fitting, 60% reported only a mild tingling sensation during stimulation. Overall, all participants found the taVNS delivered through the hydrogel earbud electrodes to be tolerable (n=6) or very tolerable (n=14). This favorable safety profile supports the potential for integrating this non-pharmacological tool into clinical breast cancer care.
Significant Improvements in Sleep and Mental Health
The primary hypothesis that nightly taVNS would safely improve sleep quality and reduce insomnia severity was supported by both subjective patient-reported outcomes and objective biometrics.
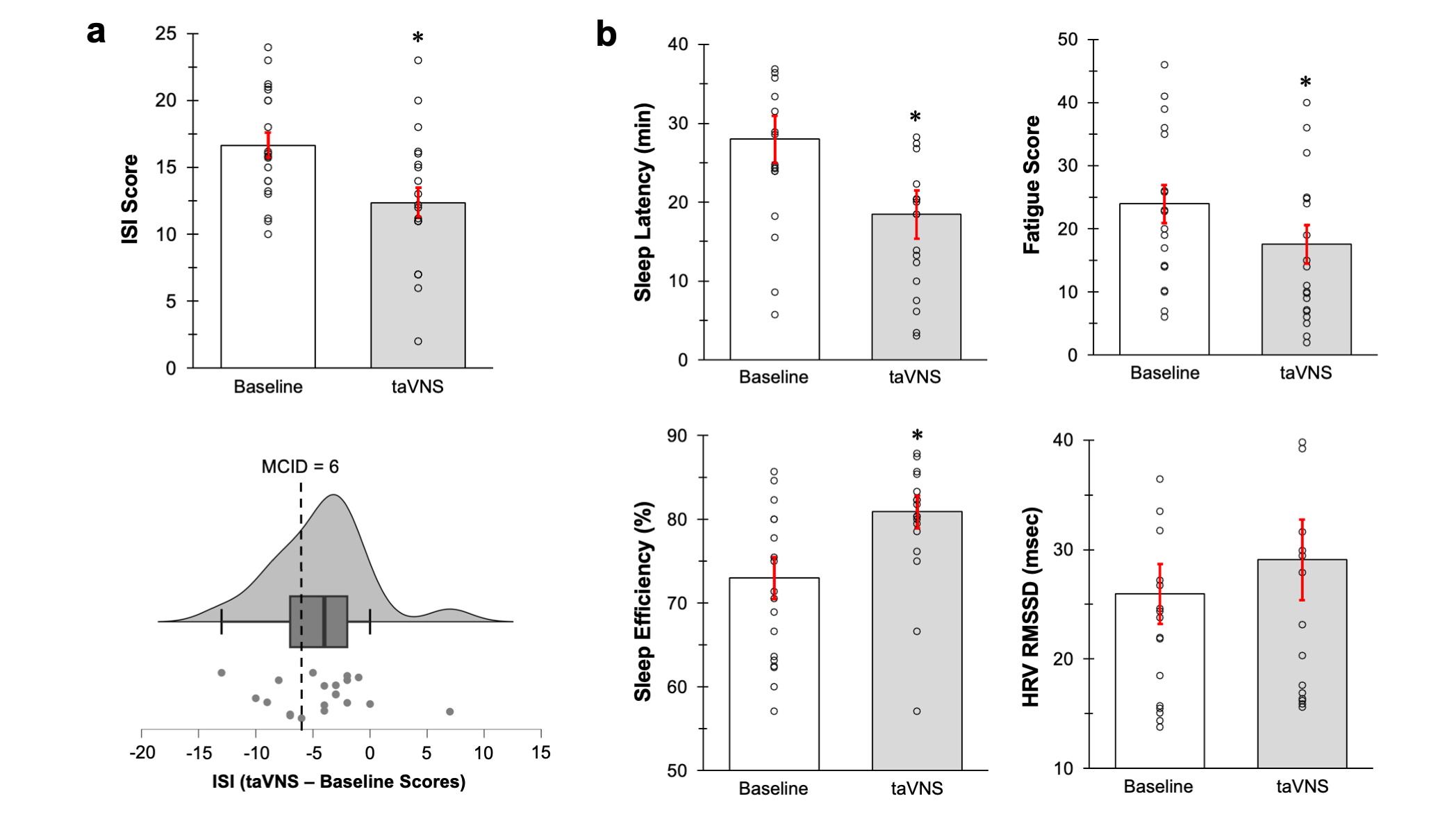
Subjective Outcomes: At baseline, participants exhibited moderate to severe insomnia (Insomnia Severity Index (ISI) score of 16.65) and poor sleep quality (Pittsburgh Sleep Quality Index (PSQI) score of 11.2). Following two weeks of treatment, taVNS produced a significant reduction in ISI (Figure 2) [2].
Objective Biometrics and Autonomic Function: Objective measures using nightly actigraphy and heart rate photoplethysmography (PPG) confirmed significant improvements in sleep architecture. We found taVNS produced a significant reduction in sleep onset latency (the time taken to fall asleep) and a significant improvement in sleep efficiency (Figure 2) [2]. Furthermore, there was a significant decrease in the number of nightly awakenings compared to baseline. These improvements in objective sleep quality were evident within just the first week of taVNS treatment.
The intervention also positively modulated the autonomic nervous system, a key regulator of physical and psychological health. We found taVNS produced a significant increase in Heart Rate Variability (HRV), specifically measured by the root mean square of successive differences (RMSSD) during sleep. Higher HRV is widely recognized as a marker of reduced sympathetic arousal, increased vagal tone, and enhanced physiological resilience to stress.
Mental Health and Fatigue: Beyond sleep, the treatment significantly addressed associated comorbidities. We found taVNS yielded very strong evidence for a significant 27% reduction in cancer-related fatigue (CFS) scores, a major complaint among breast cancer patients [2]. Mild depression scores (PHQ-9) were also significantly reduced by 26% [2]. Although anxiety symptoms were mild at baseline, the treatment produced a slight, non-significant reduction in anxiety scores. These data collectively provide strong preliminary evidence that taVNS can improve depression and fatigue, potentially by enhancing sleep quality.
Proposed Neurobiological Mechanisms
The efficacy of taVNS is hypothesized to stem from its modulatory action on two interconnected regulatory systems: the locus coeruleus-norepinephrine (LC-NE) system and the cholinergic anti-inflammatory pathway (CAIP).
- LC-NE Modulation and Arousal: Stimulation of the ABVN is known to activate structures along the vagal afferent pathway and modulate ascending arousal pathways, including the LC-NE system, which is crucial for regulating alertness, mood, attention, and sleep/wake cycles. Researchers suggest that taVNS may facilitate sleep onset by promoting a clonidine-like action mediated through alpha-2-adrenergic receptors. This action reduces tonic activity in LC neurons, thereby reducing sympathetic activity and promoting sleep onset.
- Anti-Inflammatory Effects: Chronic inflammation is a significant contributor to sleep disturbances, fatigue, and diminished quality of life in cancer survivors. The vagus nerve plays a critical role in inflammatory reflexes. Vagus nerve stimulation activates the CAIP, which suppresses systemic inflammation by reducing pro-inflammatory cytokines such as TNF-, IL-1, and IL-6, whose elevation is associated with disrupted sleep, increased fatigue, and poorer cancer prognosis. The observed increase in HRV in this study supports enhanced autonomic regulation, which is consistent with the activation of anti-inflammatory pathways.
Future Directions and Scalability
The use of comfortable, conductive hydrogel earbud electrodes (BRAIN Buds) advances taVNS methods, improving the scalability and ease of integration of this non-pharmacological approach [1]. Given that cancer centers often fail to routinely screen for sleep disorders, an accessible, low-burden intervention like taVNS holds strong potential to address pressing health concerns and improve the quality of life for cancer survivors.
However, the current observations are derived from an open-label pilot study with a modest sample size. To fully validate these findings and translate them into clinical practice, future investigations must prioritize multi-site, randomized, placebo-controlled trials with longer study periods. These larger studies should also aim to define optimal dosing parameters and incorporate more precise, clinical-grade physiological monitoring such as electrode-based ECG and polysomnography to definitively delineate the temporal effects and mechanisms of action, especially concerning the interplay between LC-NE signaling, inflammation, and sleep regulation in this patient population. Overall, these studies demonstrate that taVNS delivered via a familiar earbud form factor is a promising and feasible approach to improving sleep, mood, and health for women battling breast cancer and chronic insomnia.
References
1. Tyler, William J. "Auricular bioelectronic devices for health, medicine, and human-computer interfaces." Frontiers in Electronics 6 (2025): 1503425.
2. Do, M., Evancho, A. & Tyler, W.J. Bilateral transcutaneous auricular vagus nerve stimulation for the treatment of insomnia in breast cancer. Sci Rep (2025). https://doi.org/10.1038/s41598-025-30600-6
Follow the Topic
-
Scientific Reports

An open access journal publishing original research from across all areas of the natural sciences, psychology, medicine and engineering.
Related Collections
With Collections, you can get published faster and increase your visibility.
Obesity
Publishing Model: Hybrid
Deadline: Apr 24, 2026
Reproductive Health
Publishing Model: Hybrid
Deadline: Mar 30, 2026
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in