Why we studied diabetes screening uptake in Aceh, Indonesia
Published in Healthcare & Nursing, Social Sciences, and General & Internal Medicine

The story behind the research

When we started our research project in 2019, the ambition of Indonesia’s health system was clear: free, community-based screening services for noncommunicable diseases (NCDs) such as hypertension and diabetes were rolled out broadly — every community health center (“Puskesmas”) and many village level “Posbindu” (health posts) offered screening. Yet, uptake remained surprisingly low.
We began asking: why? If the financial and logistical barriers are largely addressed (i.e. screenings are free and local), what holds people back from actually going? Are there knowledge gaps? Misconceptions? Attitudes that deter action? And how much does socioeconomic status or education play a role in who gets screened?
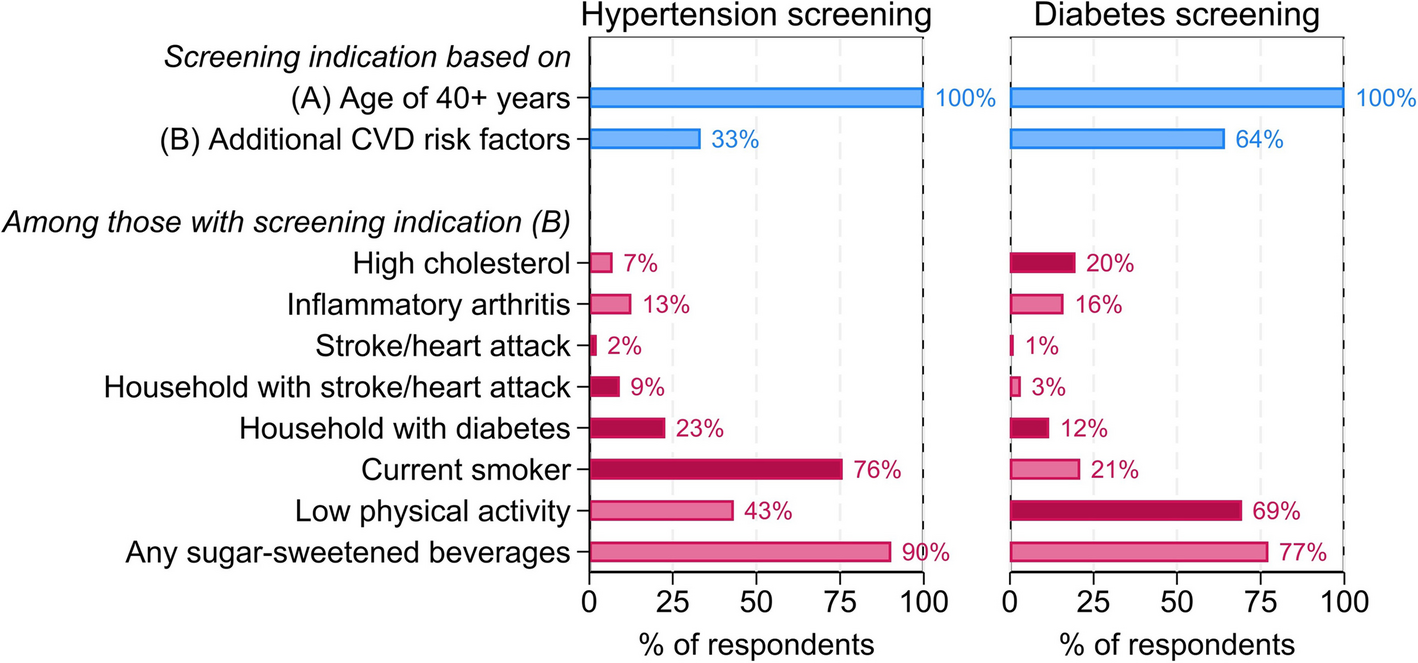
Our aim was to probe these barriers, from the perspective of the individuals—their knowledge, beliefs, and behaviors (KAP)—in a representative sample of adults aged 40–70 who should be screened per WHO PEN guidelines but who had not been recently screened. We believed that a deeper understanding of these “demand-side” obstacles could inform better strategies to close the gap in screening uptake, beyond just increasing supply.
Our approach
To explore these questions, we conducted a cross-sectional, population-based survey across the Indonesian province of Aceh in our paper "Hypertension and diabetes screening uptake in adults aged 40–70 in Indonesia: a knowledge, attitudes, and practices study". Using a two-stage cluster random sampling design, we selected 152 villages to capture a mix of urban and rural contexts and recruited adults aged 40 to 70 years — the target group for hypertension and diabetes screening under national guidelines. The study ultimately included 2,080 respondents, providing one of the largest datasets to date on community-level NCD screening behavior in Indonesia.
Data were collected through structured face-to-face interviews led by trained local enumerators. The questionnaire, adapted from WHO’s STEPS framework and national health surveys, captured four domains:
- Sociodemographic characteristics (e.g., education, income, residence);
- Knowledge of hypertension and diabetes risk factors and screening needs;
- Attitudes toward preventive screening and perceived personal risk; and
- Practices related to past screening experiences and health-seeking behaviors.
What stood out to us most
One of the most striking findings was that about 41% of respondents had never had any blood pressure or glucose check—despite free, local screening availability. Whenever respondents had been screened before, blood pressure checks were far more common than glucose checks: nearly everybody had a blood pressure measurement, but only ~21% had a blood glucose check in their last screening. That suggests that hypertension screening may be more opportunistically integrated into health encounters. In contrast, glucose testing often requires more resources, lab support, or is treated as a conditional add-on, not standard care.
We found critical gaps in the understanding of diabetes and hypertension: while most respondents were aware of these conditions, many did not know about which lifestyles may lead to diabetes and hypertension nor that they can start off ‘silently’ – without any symptoms. Instead, it was commonly believed that only those feeling ill should undergo screening.
We also saw clear socioeconomic gradients: living in rural areas, having lower education, and being in lower wealth quintiles were all strongly associated with lower knowledge and lower screening uptake. It reinforced our belief that universal access alone is not sufficient; equity in health demands addressing awareness, beliefs, and social determinants.
What this means going forward
From our work, several actionable lessons emerge:
-
Make screening guidelines and risk messaging more salient
Many people don’t see screening as relevant unless symptoms arise. Health education campaigns need to stress that hypertension and diabetes can be “silent” and that people without symptoms should still be screened. -
Differentiate strategies for hypertension vs. diabetes
The barriers appear disease‐specific—blood pressure measurements seem more normalized in care contexts, while glucose testing is rarely routine. Tailored strategies may be needed for each, including that health systems could equip more frontline facilities with affordable point-of-care glucose devices and protocols. -
Leverage trusted community platforms
Posbindu screening posts were underutilized (only 9% of last screenings) despite being very local. Strengthening their visibility, reducing resource constraints, and reframing usage so people don’t dismiss them as for “the elderly only” could help. -
Target disadvantaged groups with additional support
Lower-educated, rural, and lower-wealth individuals lag in both knowledge and uptake. Interventions (e.g. community outreach, peer education, mobile reminders) should especially prioritize those groups.
We hope our work helps health planners in Indonesia — and other settings with persistent gaps in NCD screening — in their efforts to holistically bridge the last mile: not just offering services, but ensuring they are seen, understood, trusted, and accessible by everyone. While there are some evidence-based approaches on how to achieve this (also see our paper on the effect of SMS reminders on diabetes and hypertension screening uptake in the same study population), more large-scale, effective, and innovative ideas are needed to ensure NCD care for all!
Follow the Topic
-
BMC Global and Public Health

An open access, transparent peer review journal publishing outstanding and influential research and opinion of broad interest to all professional communities involved in global and public health research, policy-making, implementation and delivery worldwide.
Related Collections
With Collections, you can get published faster and increase your visibility.
Understanding the HIV care continuum: Progress and challenges
BMC Global and Public Health is calling for submissions to our Collection on understanding the complexities and advancements in global health frameworks. This Collection will highlight key findings and challenges in maintaining continuity of care for populations affected by HIV across diverse regions.
This Collection aims to explore the multifaceted nature of HIV care, examining the ongoing challenges and recent advances in care delivery systems. We welcome contributions that offer a comprehensive understanding of how access to care, quality of treatment, and sustained engagement with healthcare systems impact health outcomes for individuals living with HIV.
Potential topics include but are not limited to:
The role of diagnosis and early detection in improving long-term health outcomes
Strategies for improving linkage to care and retention in care
The impact of antiretroviral therapy in managing HIV
Barriers to viral suppression and achieving optimal care continuity
Innovations in pre-exposure prophylaxis (PrEP) for at-risk populations
The influence of socioeconomic, cultural, and political factors on HIV care accessibility
This Collection aims to contribute to a more thorough and collaborative understanding of HIV care challenges worldwide, focusing on solutions and the pathways needed to support people living with HIV, ensuring their access to effective, ongoing care. We look forward to receiving innovative and impactful research that will push the boundaries of our current knowledge.
We encourage work from local, regional, national, and global partnerships and collaboration among multidisciplinary scientists using multiple methodologies. We ask that authors be careful to use non-stigmatizing/preferred language in their manuscripts as outlined in relevant language guidelines for their respective fields.
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Mar 18, 2026
Ensuring equality in vaccine access: Addressing global inadequacies
BMC Global and Public Health is calling for submissions to our Collection on ensuring equality in vaccine access and addressing global inadequacies. In light of current global health challenges and recurring public health emergencies, equitable vaccine allocation has emerged as a critical issue that demands urgent attention. Disparities in access to vaccines highlight systemic inequalities that hinder efforts to achieve global health security and promote health equity.
This Collection aims to showcase cutting-edge research examining the multifaceted barriers to vaccine access and strategies to overcome them. We invite contributions that explore innovative approaches, evidence-based interventions, policy analyses, and community engagement efforts aimed at promoting equitable vaccine distribution worldwide. This Collection supports and amplifies research related to:
Social determinants of vaccine access
Community engagement in vaccine implementation
Global partnerships for equitable vaccine allocation and distribution
Policy interventions to address vaccine inequities
Initiatives to fast-track vaccine R&D
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 10: Reduced Inequalities.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Mar 19, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in