Successful weaning from parenteral nutrition in a short bowel syndrome patient with high-output stoma through restricted oral diet: a case report
Published in Healthcare & Nursing, General & Internal Medicine, and Pharmacy & Pharmacology
Understanding Short Bowel Syndrome and High-Output Stomas
Short Bowel Syndrome (SBS) is a clinical condition with a small bowel remnant in continuity less than 200 cm, due to a surgical resection [1]. This condition significantly impairs the body's ability to absorb nutrients, fluids, and electrolytes, leading to severe malnutrition and dehydration [1]. SBS patients often experience increased intestinal output, particularly if they are classified as net “secretors” (usually having less than 100 cm residual jejunum), meaning that they lose more water and sodium from their stoma than they take by mouth [2, 3].
The Case Study
The case of a 67-year-old woman, who suffered from SBS after extensive surgical interventions, serves as a powerful example of how tailored nutrition can improve patient's condition. The patient had a medical history that included multiple surgeries due to ulcerative colitis, neurofibromatosis type 1, and rheumatoid arthritis. In 2023, after experiencing complications from an anastomosis leak, she underwent an extensive enterectomy, leaving her with just 80 cm of small bowel and an end-jejunostomy. Her weight had dropped to a critical 50 kg, a 12% loss from her previous 57 kg, indicating severe malnutrition.
The Role of a Restricted Oral Diet in Managing SBS
Patients with SBS, particularly those with high-output stomas, must manage their fluid and nutrient intake meticulously. For the 67-year-old patient, her nutritional regimen began with a liquid diet and was carefully adjusted over time to include a residue-free regimen with added salt. She was also advised to limit her fluid intake to less than one liter per day, supplemented with oral rehydration solutions.
Despite these efforts, her stoma output remained elevated, and additional medications such as loperamide were introduced to reduce intestinal transit time and stoma output. The nutritional care team found the optimal balance: a restricted oral intake of 1000 to 1200 kcal/day, combined with parenteral nutrition (PN) and strict fluid management.
Gradual Improvement
Three months after her surgery, the patient’s condition began to stabilize. Her stoma output dropped to 1.4-1.8 liters per day, and her weight fluctuated between 50.4 and 50.8 kg. To further enhance her treatment, teduglutide, a medication used to improve intestinal absorption, was introduced, at 0.1 mg/kg/day, along with an unrestricted oral diet. After incorporating teduglutide into her treatment plan, the patient’s stoma output remained stable at 1.3 to 1.5 liters per day, and she managed to gain weight, reaching 52 kg by the time of discharge. Her grip strength also improved, further indicating her recovery from malnutrition (Fig. 1).
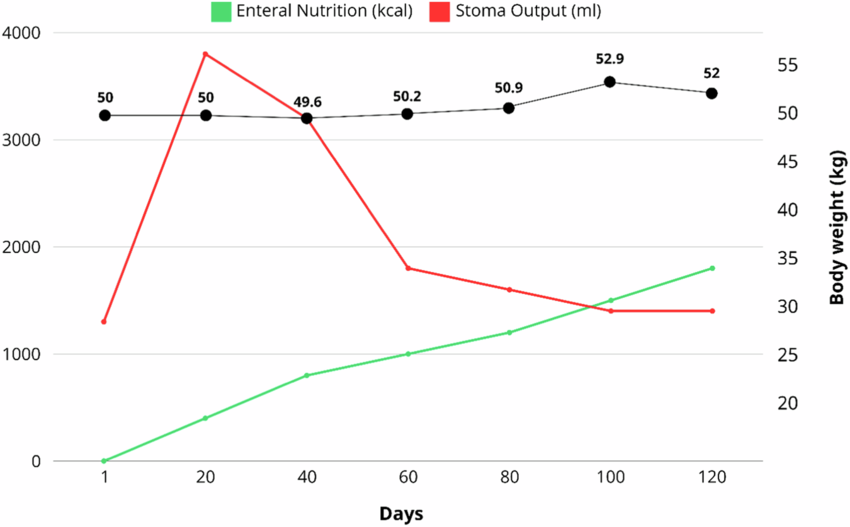
Figure 1. Changes in Enteral Nutrition intake, stoma output and body weight after end-jejunostomy.
The patient stayed in the hospital for four months and was successfully weaned off PN, transitioning to an unrestricted oral diet. Upon discharge, she was relying on an oral diet with specific nutritional recommendations and parenteral saline.
Key takeaways
- A tailored restrictive oral diet significantly reduced stoma output and improved the patient's nutritional status.
- High patient compliance and a multidisciplinary approach were essential in achieving successful weaning from parenteral nutrition.
- Pharmacological advancements, including the use of Teduglutide, demonstrated promising results in improving intestinal absorption and patient outcomes.
References
1. Pironi L, Cuerda C, Jeppesen PB, Joly F, Jonkers C, Krznarić Ž, et al. ESPEN guideline on chronic intestinal failure in adults - Update 2023. Clin Nutr. 2023;42:1940–2021. https://doi.org/10.1016/j.clnu.2023.07.019
2. Klek S, Forbes A, Gabe S, Holst M, Wanten G, Irtun Ø, et al. Management of acute intestinal failure: a position paper from the European Society for Clinical Nutrition and Metabolism (ESPEN) Special Interest Group. Clin Nutr. 2016;35:1209–18. https://doi.org/10.1016/j.clnu.2016.04.009
3. Nightingale J, Woodward JM. Small Bowel and nutrition committee of the British Society of Gastroenterology. Guidelines for management of patients with a short bowel. Gut. 2006;55:Suppl 4–iv12. https://doi.org/10.1136/gut.2006.091108
Follow the Topic
-
European Journal of Clinical Nutrition

An international, peer-reviewed journal covering all aspects of human and clinical nutrition. This may encompass clinical, metabolic and epidemiological studies that describe nutritional interventions for clinical disease and health promotion.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in