A consensus statement for digital surgery
Published in Healthcare & Nursing
Explore the Research
A Delphi consensus statement for digital surgery - npj Digital Medicine
npj Digital Medicine - A Delphi consensus statement for digital surgery
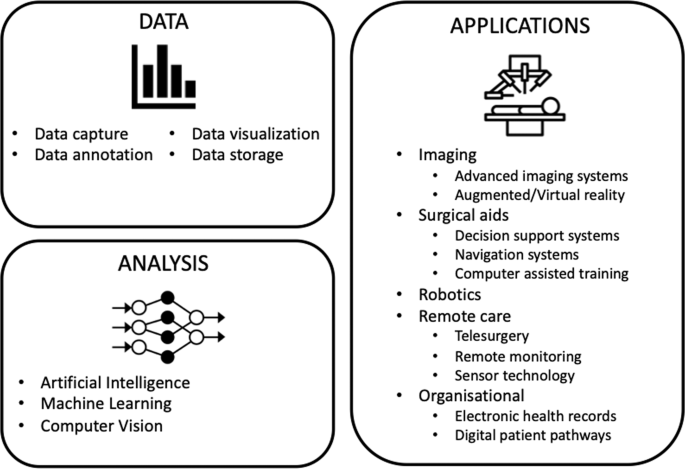
Digital technology is being rapidly adopted in surgery. A variety of technologies ranging from robotics1, advanced imaging systems2, and artificial intelligence3 offer surgeons and their teams the promise of increased efficiency, improved performance and ultimately better patient outcomes4,5. A significant driver behind this uptake in digital technology within the operating room has been the commercial opportunity it offers. Surgical robotics makes up only a proportion of these technologies yet is valued at $5 billion and estimated to continue growing6.
The use of digital technology within surgery, however, is not unique to surgery; digital technology has been widely implemented across healthcare. However, we argue that this specific focus on digital surgery is necessary for a number of reasons. Firstly, digital surgery is a term that has been widely used within the specialty, despite the meaning of the term being unclear. Standardisation of this terminology is required for safe and effective translation of this technology into clinical practice; it is impossible to quality assure clinical interventions or trials without this. It is also essential that digital surgery can be explained to patients clearly and consistently especially in the context of data collection and processing. Secondly, this lack of clarity surrounding digital surgery impedes process. In rapidly emerging fields, such as digital surgery, there is a need for research priorities and areas for collaboration to be clearly identified. Finally, surgery is a high-risk clinical intervention when compared to other medical use cases with the potential to cause serious patient harm.
Digital surgery may also pose unique challenges not found across wider digital health. For example, privacy concerns extend beyond the patient, normally the sole concern within digital health applications, to the surgeon and their team who may be scrutinised for their potential actions within the operating room. Furthermore, this concern may not only hinder deployment of digital surgery but also its development as surgical teams worry how donated data may potentially be used for other purposes such as litigation. The potential benefits of digital surgery may cause such challenges to be easily overlooked. We therefore aimed to define the term digital surgery, identify these key challenges and propose future research goals within this field.
Given the limited evidence within this field and the need for knowledge to be drawn from multiple areas of expertise, we chose to implement Delphi methodology7. It has previously been successfully used to determine consensus in varying areas across healthcare8,9. It consists of multiple iterative voting rounds where panelists are able to review the group’s votes, propose new items and ultimately converge towards consensus. In our Delphi, 38 international experts across the fields of surgery, technology, industry, law, ethics, and health policy undertook a 4 round Delphi (Figure 1). An initial scoping round, which was conducted in conjunction with a public panel, allowed issues to be generated which were subsequently voted upon in two subsequent voting rounds before all items were discussed in a final online consensus meeting.
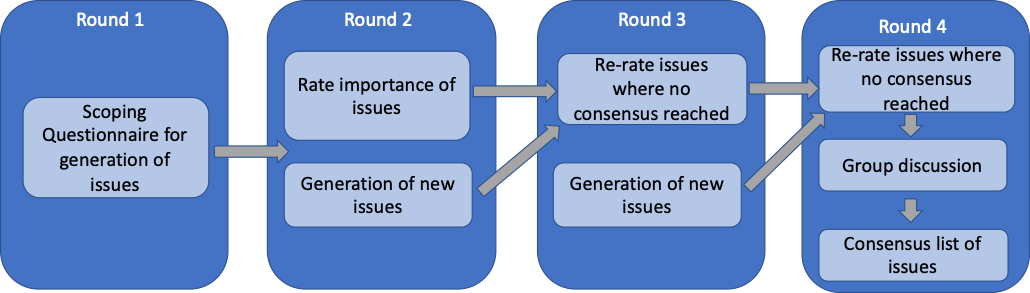
Consensus was obtained across 114 issues which were divided into 7 key areas: definition of digital surgery; data; privacy, confidentiality and public trust; consent; law; litigation and liability; and commercial partnerships. 38 barriers associated with the development, deployment and monitoring of digital surgery and 22 future research goals were identified and ranked with respect to their importance.
Digital surgery was defined as the use of technology for the enhancement of preoperative planning, surgical performance, therapeutic support, or training, to improve outcomes and reduce harm.
Three main themes can be drawn upon from the issues highlighted. Firstly, the current lack of infrastructure within hospitals to support digital surgery. The majority of operating rooms lack the technical infrastructure to routinely record data hindering the development and adoption of digital surgery. Secondly, there is a need for patient and public engagement to ensure ethical and trustworthy digital surgery. Patients and the public must be aware of what they are consenting to when donating their data. Finally, appropriate education should be provided for all stakeholders within digital surgery. We argue that the future digital surgeon must not be a surgeon in isolation; they must understand the technical basis of the technology they are using and be aware of the legal, ethical and data governance issues concerning its use.
Overall, this study achieves consensus definition of the term digital surgery. We highlight key issues concerning digital surgery and identify barriers and future research goals within the field which will act as a platform for future research.
References
- Kinross, J. M., Mason, S. E., Mylonas, G. & Darzi, A. Next-generation robotics in gastrointestinal surgery. Nature Reviews Gastroenterology & Hepatology 17, 430-440, 658 doi:10.1038/s41575-020-0290-z (2020).
- Tepper, O. M. et al. Mixed Reality with HoloLens: Where Virtual Reality Meets Augmented Reality in the Operating Room. Plast Reconstr Surg 140, 1066-1070, doi:10.1097/prs.0000000000003802 (2017).
- Hashimoto, D. A., Rosman, G., Rus, D. & Meireles, O. R. Artificial Intelligence in Surgery: Promises and Perils. Ann Surg 268, 70-76, doi:10.1097/sla.0000000000002693 (2018).
- Maier-Hein, L. et al. Surgical data science - from concepts toward clinical translation. Med Image Anal 76, 102306, doi:10.1016/j.media.2021.102306 (2022).
- Maier-Hein, L. et al. Surgical data science for next-generation interventions. Nature Biomedical Engineering 1, 691-696, doi:10.1038/s41551-017-0132-7 (2017).
- Research and Markets. Global Surgical Robotics Market 2021-2031: Focus on Vendor Analysis, Key Enabling Technologies, Emerging Platforms in Pipeline, 26 Company Profiles, and 45 Countries Data & Cross Segmentation <https://www.researchandmarkets.com/reports/5318090/global-surgical-robotics-market 2021-2031-focus>
- Hasson, F., Keeney, S. & McKenna, H. Research guidelines for the Delphi survey technique. Journal of Advanced Nursing 32, 1008-1015, doi:https://doi.org/10.1046/j.1365- 709 2648.2000.t01-1-01567.x (2000).
- DʼSouza, N. et al. Definition of the Rectum: An International, Expert-based Delphi Consensus. Ann Surg 270, 955-959, doi:10.1097/sla.0000000000003251 (2019).
- Ferguson, N. D., Davis, A. M., Slutsky, A. S. & Stewart, T. E. Development of a clinical definition for acute respiratory distress syndrome using the Delphi technique. J Crit Care 20, 147-154, doi:10.1016/j.jcrc.2005.03.001 (2005).
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in