A Genomic Wake-Up Call: Rethinking Breast Cancer Through the African Lens
Published in Cancer and Genetics & Genomics
Breast cancer is one of the top causes of death for women in Africa. But scientists still don’t know enough about how the disease works in African women. Most of the big studies on cancer have looked at people from Europe or North America. This means we don’t have enough information about how breast cancer affects women in other parts of the world—especially Africa.
In a recent study published in NPJ Breast Cancer, our team looked at all the research so far on breast cancer genes in African women. We found some important differences in their tumors compared to people from other backgrounds. These differences might help us figure out better ways to treat cancer in the future. But they also show how much we still need to learn.
In this blog post, we’ll explain what we found and why it matters for cancer care around the world.
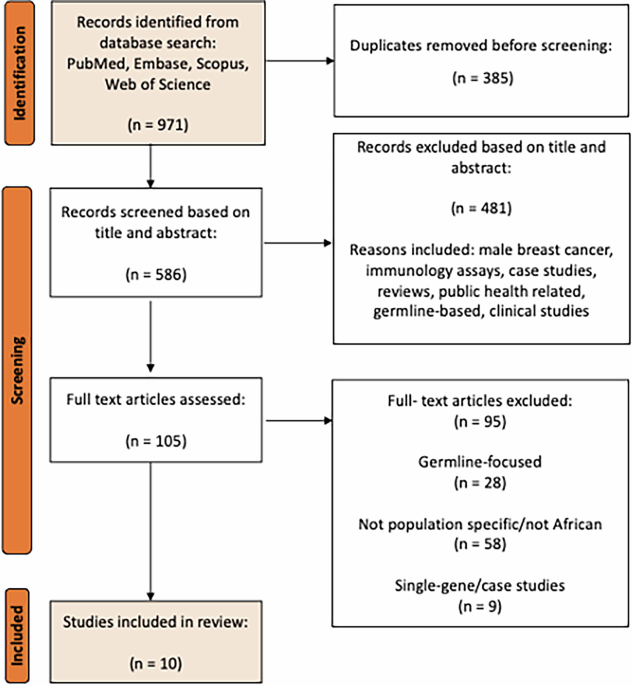
What We Did
We looked at 10 research studies from seven African countries, including Nigeria, Egypt, Kenya, Tunisia, Mali, Ethiopia, and Ghana. These studies looked at the DNA of breast cancer tumors using modern lab tools. In total, the studies included over 500 women. Even though we searched a lot of papers from 2004 to 2024, only a small number of countries in Africa had published this kind of research. Most of the data came from Nigeria.
What We Found
We noticed some key differences in the cancer genes of African women. One important gene, called TP53, was found to be changed (or mutated) more often in African women than in people from other backgrounds. This gene is known to make cancers more aggressive. Another gene, called PIK3CA, was less likely to be mutated in African women. This is important because some cancer treatments are made to target this gene, so they might not work as well in African patients.
We also found that many of the African tumors had a high number of mutations in general. This is called a “high tumor mutational burden,” or TMB. It might make some of these cancers respond better to a type of medicine called immunotherapy, which helps the immune system fight cancer. However, these treatments are not widely available in most African countries.
New Genes and Differences in DNA Structure
Some studies found genes that had never been linked to breast cancer before. These include PLK2, GPD2, and TDRD15. Some of these genes showed up more often in certain types of breast cancer, like HER2-positive tumors. These findings are exciting, but the number of patients was small. We’ll need more research to know for sure what these genes mean.
We also looked at changes in the number of copies of certain genes, known as “copy number alterations.” In some African tumors, there were more copies of genes like EZH2 and ERBB2. In other cases, important genes like TP53 were missing altogether. These changes can affect how cancer grows and how it responds to treatment.
Patterns in Mutations
We also studied something called “mutational signatures.” These are patterns in the DNA that can tell us what might have caused the cancer. One pattern, linked to a problem called homologous recombination deficiency (HRD), was seen more often in Nigerian patients. This may mean that certain drugs—like PARP inhibitors—could help some of these patients.
What We Still Don’t Know
Even though we found some important clues, there’s still a lot we don’t understand. We don’t yet know exactly why African tumors look so different. Is it because of genetics? The environment? Or because many women are diagnosed late, when the cancer is already advanced? Right now, we don’t have enough information to say for sure.
Africa is also one of the most genetically diverse places in the world, with over 2,000 different ethnic groups. But most studies don’t take this into account. To really understand what’s going on, we need more research that looks at different populations, types of cancer, and patient histories.
What Needs to Happen Next
Our study shows how important it is to invest in cancer research in Africa. This means setting up better labs, collecting samples, training scientists, and making sure the research is led by African experts. It’s also important that these discoveries lead to real improvements in cancer care—like tests and treatments that are affordable and work well for African women.
As cancer treatment becomes more focused on the individual, we must make sure no one is left behind. Studying African genomes isn’t just about fairness—it can also help all of us understand cancer better. These unique patterns in African tumors could unlock new ways to treat the disease around the world.
This is a call for more inclusive science. Global problems need global answers.
If you want to dive deeper, you can find the paper here Genomic landscapes of breast cancer in African populations: a systematic review | npj Breast Cancer
Follow the Topic
-
npj Breast Cancer

This journal publishes original research articles, reviews, brief communications, matters arising, meeting reports and hypothesis generating observations which could be unexplained or preliminary findings from experiments, novel ideas or the framing of new questions that need to be solved.
Related Collections
With Collections, you can get published faster and increase your visibility.
Molecular Tumor Board in Breast Cancer
Publishing Model: Open Access
Deadline: Jul 22, 2026
Rare breast cancer subtypes
Publishing Model: Open Access
Deadline: Mar 24, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in