Altered Striatal Phosphodiesterase 10A in Bipolar I Disorder: A Step Toward Understanding Mood Recurrence
Published in Neuroscience and General & Internal Medicine
Bipolar I disorder (BD-I) is a complex psychiatric condition characterized by recurrent episodes of mania and depression. Despite ongoing research, the precise mechanisms behind the recurrence of these mood episodes remain unclear. A recent study led by Keisuke Takahata and Yasuharu Yamamoto and their team provides valuable insights into the role of phosphodiesterase 10A (PDE10A) in BD-I, suggesting it may be key to understanding the disorder's mood instability.
This study, published in Translational Psychiatry, is the first of its kind to explore the alterations of PDE10A in the brains of individuals with BD-I, highlighting a potential pathway that could explain the frequent mood swings seen in these patients. The findings are promising, potentially laying the groundwork for new therapeutic strategies aimed at preventing episode recurrence in BD-I.
The Study: Striatal PDE10A and Mood Episodes in BD-I
The primary objective of the study was to assess whether striatal PDE10A availability was altered in patients with BD-I compared to healthy controls and to examine the relationship between these alterations and the clinical characteristics of BD-I. This was achieved using positron emission tomography (PET) scans with a radioligand that binds to PDE10A, providing a detailed view of its availability in different regions of the brain.
We focused on the striatum, a brain region known for its involvement in regulating mood, cognition, and motor control. The study included 25 patients diagnosed with BD-I and 27 age- and sex-matched healthy controls. Importantly, most of the BD-I patients were in a euthymic state, meaning they were not currently experiencing manic or depressive episodes, allowing the researchers to focus on trait-related changes rather than state-dependent effects.
![Representative [18F]MNI-659 BPND parametric and ROI images.](https://images.zapnito.com/cdn-cgi/image/metadata=copyright,format=auto,quality=95,fit=scale-down/https://images.zapnito.com/uploads/KmzJ55RqTqS2nnrW9G57_figure1.jpg)
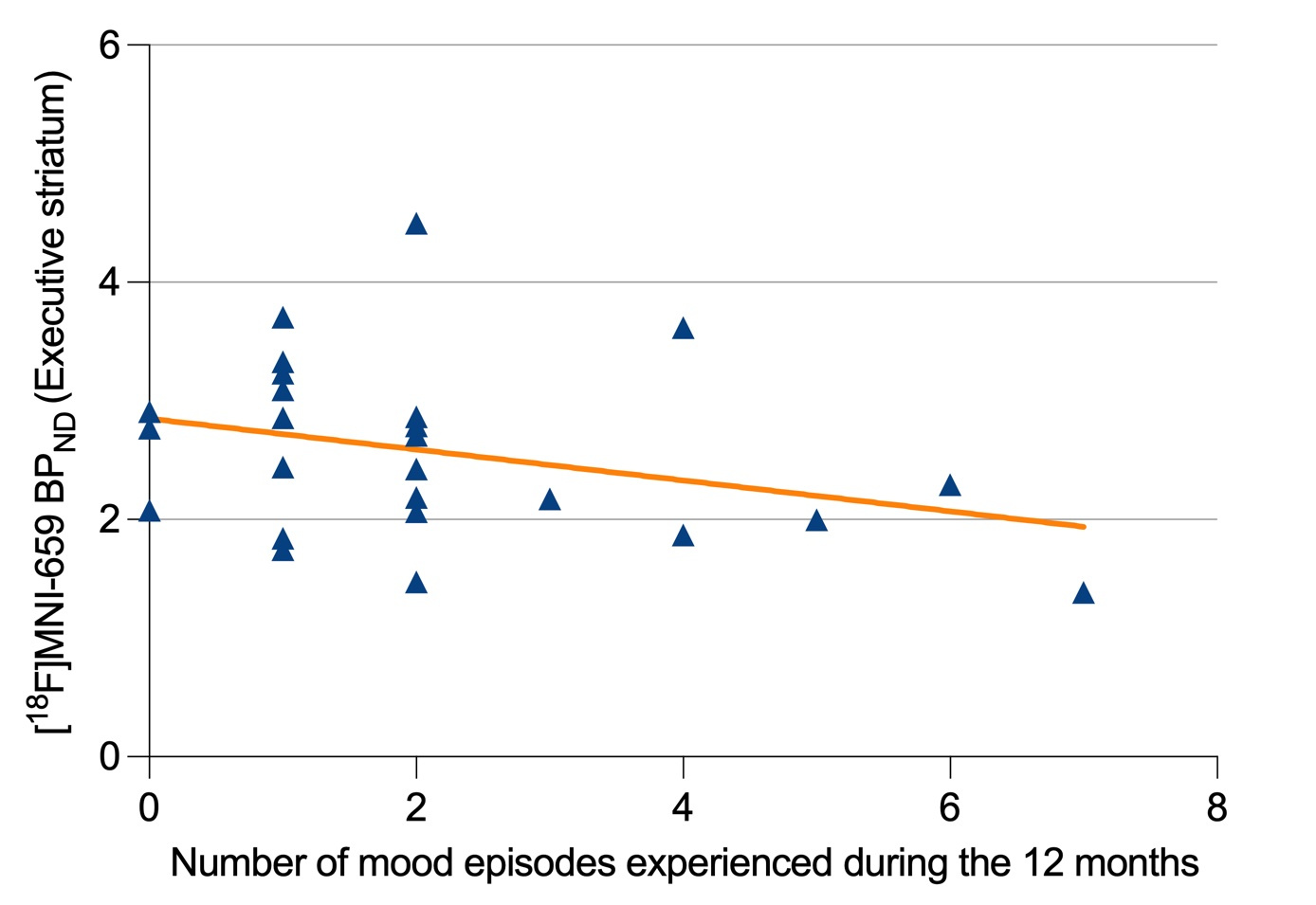
The key finding was that patients with BD-I had significantly lower PDE10A availability in two subregions of the striatum: the executive and sensorimotor areas. The executive subregion, in particular, showed a strong correlation between reduced PDE10A levels and a higher number of mood episodes in the past year. This suggests that diminished PDE10A activity in this area could be linked to a greater risk of recurrent mood episodes, making it a critical area of focus for future research.
![[18F]MNI-659 BPND in the striatal subregions of patients with BD-I and healthy controls.](https://images.zapnito.com/cdn-cgi/image/metadata=copyright,format=auto,quality=95,fit=scale-down/https://images.zapnito.com/uploads/JsY4JcEET62BAfe8A0Cw_figure2.jpg)
 Why PDE10A?
Why PDE10A?
PDE10A plays a crucial role in the second messenger signaling downstream of dopamine receptor activation, making it a key regulator of dopamine transmission in the brain. Given that dopamine is heavily implicated in mood regulation, it stands to reason that alterations in PDE10A could contribute to the dysregulation of mood seen in BD-I.
Previous research has hinted at the involvement of dopamine in BD-I, with studies showing that medications targeting dopamine, such as antipsychotics, are effective in reducing the recurrence of mood episodes. However, the results from earlier PET studies examining dopamine signaling in BD-I have been inconsistent. By focusing on PDE10A, a downstream regulator of dopamine signaling, the present study offers a fresh perspective on how dopamine dysfunction may contribute to the pathophysiology of BD-I.
The reduced PDE10A availability observed in BD-I patients suggests that the enzyme may be less effective at breaking down cyclic adenosine monophosphate (cAMP), a critical signaling molecule in dopamine pathways. This could lead to a prolonged and dysregulated dopamine signal, contributing to the mood instability characteristic of BD-I.
Clinical Implications and Future Directions
One of the most significant implications of this study is the potential for targeting PDE10A as a therapeutic strategy for preventing relapse in BD-I. If reduced PDE10A availability is indeed contributing to the recurrence of mood episodes, then drugs designed to boost PDE10A activity could help stabilize mood in BD-I patients and reduce the frequency of their episodes.
Interestingly, the study also found that the reduction in PDE10A availability was not uniform across the entire striatum. The executive and sensorimotor subregions were most affected, while the limbic subregion, which is often associated with emotion and motivation, showed no significant differences between BD-I patients and healthy controls. This suggests that the cognitive aspects of BD-I, such as difficulties with decision-making and working memory, may be more closely tied to PDE10A dysfunction than the emotional aspects of the disorder.
Despite the promising findings, the authors acknowledge several limitations. The sample size was relatively small, and most of the BD-I patients were in a euthymic state, limiting the ability to examine PDE10A alterations during manic or depressive episodes. Additionally, while the study found a strong correlation between reduced PDE10A availability and the frequency of mood episodes, it could not establish a direct causal relationship. Future longitudinal studies are needed to confirm whether PDE10A dysfunction directly contributes to the onset of mood episodes or is a consequence of other pathological processes in BD-I.
The study also opens the door to exploring PDE10A in other psychiatric conditions. For instance, recent research has shown that PDE10A availability is increased in patients with schizophrenia, another disorder characterized by dopamine dysregulation. This raises the intriguing possibility that PDE10A may function differently across various psychiatric conditions, offering a potential biomarker to distinguish between disorders like BD-I and schizophrenia.
Conclusion
This groundbreaking study provides the first direct evidence of altered PDE10A availability in BD-I, linking reduced PDE10A activity in the executive striatum to an increased risk of mood episode recurrence. By highlighting PDE10A as a potential target for therapeutic intervention, the research offers a new avenue for understanding and treating BD-I. As future studies build on these findings, PDE10A may become a key player in the fight against the debilitating mood swings that characterize this disorder.
The implications for treatment are significant. If PDE10A activity can be modulated with medication, it could lead to a new class of treatments for BD-I aimed not just at managing symptoms during episodes but at preventing them from occurring in the first place. With further research, targeting PDE10A may help turn the tide in the battle against BD-I, offering hope to millions of patients worldwide.
Follow the Topic
-
Translational Psychiatry

This journal focuses on papers that directly study psychiatric disorders and bring new discovery into clinical practice.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Moving towards mechanism, causality and novel therapeutic interventions in translational psychiatry: focus on the microbiome-gut-brain axis
Publishing Model: Open Access
Deadline: May 19, 2026
From mechanism to intervention: translational psychiatry of childhood maltreatment
Publishing Model: Open Access
Deadline: Feb 28, 2026






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in